Cardiovascular disease
| Cardiovascular disease | |
|---|---|
 | |
| Micrograph of a heart with fibrosis (yellow) and amyloidosis (brown). Movat's stain. | |
| Specialty | Cardiology |
| Symptoms | Chest pain, shortness of breath, fatigue, loss of consciousness |
| Complications | Heart failure, heart attack, stroke, aneurysm, peripheral artery disease, sudden cardiac arrest.[1] |
| Usual onset | Older adults[2] |
| Types | Coronary artery diseases, stroke, heart failure, hypertensive heart disease, rheumatic heart disease, cardiomyopathy,[3][4] Arrhythmia |
| Risk factors | Diabetes,[3] high blood lipids, excess weight, Smoking, excessive drug use, and excessive alcohol intake |
| Prevention | Healthy eating, exercise, avoiding tobacco smoke, limited alcohol intake,[3] Overall lifestyle changes |
| Treatment | Treating high blood pressure, high blood lipids, diabetes[3] |
| Medication | Aspirin, beta blockers, blood thinners |
| Deaths | 17.9 million / 32% (2015)[5] |
Cardiovascular disease (CVD) is any disease involving the heart or blood vessels.[3] CVDs constitute a class of diseases that includes: coronary artery diseases (e.g. angina, heart attack), heart failure, hypertensive heart disease, rheumatic heart disease, cardiomyopathy, arrhythmia, congenital heart disease, valvular heart disease, carditis, aortic aneurysms, peripheral artery disease, thromboembolic disease, and venous thrombosis.[3][4]
The underlying mechanisms vary depending on the disease.[3] It is estimated that dietary risk factors are associated with 53% of CVD deaths.[6] Coronary artery disease, stroke, and peripheral artery disease involve atherosclerosis.[3] This may be caused by high blood pressure, smoking, diabetes mellitus, lack of exercise, obesity, high blood cholesterol, poor diet, excessive alcohol consumption,[3] and poor sleep,[7][8] among other things. High blood pressure is estimated to account for approximately 13% of CVD deaths, while tobacco accounts for 9%, diabetes 6%, lack of exercise 6%, and obesity 5%.[3] Rheumatic heart disease may follow untreated strep throat.[3]
It is estimated that up to 90% of CVD may be preventable.[9][10] Prevention of CVD involves improving risk factors through: healthy eating, exercise, avoidance of tobacco smoke and limiting alcohol intake.[3] Treating risk factors, such as high blood pressure, blood lipids and diabetes is also beneficial.[3] Treating people who have strep throat with antibiotics can decrease the risk of rheumatic heart disease.[11] The use of aspirin in people who are otherwise healthy is of unclear benefit.[12][13]
Cardiovascular diseases are the leading cause of death worldwide except Africa.[3] Together CVD resulted in 17.9 million deaths (32.1%) in 2015, up from 12.3 million (25.8%) in 1990.[5][4] Deaths, at a given age, from CVD are more common and have been increasing in much of the developing world, while rates have declined in most of the developed world since the 1970s.[14][15] Coronary artery disease and stroke account for 80% of CVD deaths in males and 75% of CVD deaths in females.[3] Most cardiovascular disease affects older adults. In the United States 11% of people between 20 and 40 have CVD, while 37% between 40 and 60, 71% of people between 60 and 80, and 85% of people over 80 have CVD.[2] The average age of death from coronary artery disease in the developed world is around 80, while it is around 68 in the developing world.[14] CVD is typically diagnosed seven to ten years earlier in men than in women.[3]: 48
Types

There are many cardiovascular diseases involving the blood vessels. They are known as vascular diseases.[17]
- Coronary artery disease (coronary heart disease or ischemic heart disease)
- Peripheral arterial disease – a disease of blood vessels that supply blood to the arms and legs
- Cerebrovascular disease – a disease of blood vessels that supply blood to the brain (includes stroke)
- Renal artery stenosis
- Aortic aneurysm
There are also many cardiovascular diseases that involve the heart.
- Cardiomyopathy – diseases of cardiac muscle
- Hypertensive heart disease – diseases of the heart secondary to high blood pressure or hypertension
- Heart failure – a clinical syndrome caused by the inability of the heart to supply sufficient blood to the tissues to meet their metabolic requirements
- Pulmonary heart disease – a failure at the right side of the heart with respiratory system involvement
- Cardiac dysrhythmias – abnormalities of heart rhythm
- Inflammatory heart diseases
- Endocarditis – inflammation of the inner layer of the heart, the endocardium. The structures most commonly involved are the heart valves.
- Inflammatory cardiomegaly
- Myocarditis – inflammation of the myocardium, the muscular part of the heart, caused most often by viral infection and less often by bacterial infections, certain medications, toxins, and autoimmune disorders. It is characterized in part by infiltration of the heart by lymphocyte and monocyte types of white blood cells.
- Eosinophilic myocarditis – inflammation of the myocardium caused by pathologically activated eosinophilic white blood cells. This disorder differs from myocarditis in its causes and treatments.
- Valvular heart disease
- Congenital heart disease – heart structure malformations existing at birth
- Rheumatic heart disease – heart muscles and valves damage due to rheumatic fever caused by Streptococcus pyogenes a group A streptococcal infection.
Risk factors
There are many risk factors for heart diseases: age, sex, tobacco use, physical inactivity, non-alcoholic fatty liver disease, excessive alcohol consumption, unhealthy diet, obesity, genetic predisposition and family history of cardiovascular disease, raised blood pressure (hypertension), raised blood sugar (diabetes mellitus), raised blood cholesterol (hyperlipidemia), undiagnosed celiac disease, psychosocial factors, poverty and low educational status, air pollution, and poor sleep.[3][18][19][20][21][22] While the individual contribution of each risk factor varies between different communities or ethnic groups the overall contribution of these risk factors is very consistent.[23] Some of these risk factors, such as age, sex or family history/genetic predisposition, are immutable; however, many important cardiovascular risk factors are modifiable by lifestyle change, social change, drug treatment (for example prevention of hypertension, hyperlipidemia, and diabetes).[24] People with obesity are at increased risk of atherosclerosis of the coronary arteries.[25]
Genetics
Cardiovascular disease in a person's parents increases their risk by ~3 fold,[26] and genetics is an important risk factor for cardiovascular diseases. Genetic cardiovascular disease can occur either as a consequence of single variant (Mendelian) or polygenic influences.[27] There are more than 40 inherited cardiovascular disease that can be traced to a single disease-causing DNA variant, although these conditions are rare.[27] Most common cardiovascular diseases are non-Mendelian and are thought to be due to hundreds or thousands of genetic variants (known as single nucleotide polymorphisms), each associated with a small effect.[28][29]
Age

Age is the most important risk factor in developing cardiovascular or heart diseases, with approximately a tripling of risk with each decade of life.[30] Coronary fatty streaks can begin to form in adolescence.[31] It is estimated that 82 percent of people who die of coronary heart disease are 65 and older.[32] Simultaneously, the risk of stroke doubles every decade after age 55.[33]
Multiple explanations are proposed to explain why age increases the risk of cardiovascular/heart diseases. One of them relates to serum cholesterol level.[34] In most populations, the serum total cholesterol level increases as age increases. In men, this increase levels off around age 45 to 50 years. In women, the increase continues sharply until age 60 to 65 years.[34]
Aging is also associated with changes in the mechanical and structural properties of the vascular wall, which leads to the loss of arterial elasticity and reduced arterial compliance and may subsequently lead to coronary artery disease.[35]
Sex
Men are at greater risk of heart disease than pre-menopausal women.[30][36] Once past menopause, it has been argued that a woman's risk is similar to a man's[36] although more recent data from the WHO and UN disputes this.[30] If a female has diabetes, she is more likely to develop heart disease than a male with diabetes.[37] Women who have high blood pressure and had complications in their pregnancy have three times the risk of developing cardiovascular disease compared to women with normal blood pressure who had no complications in pregnancy.[38][39]
Coronary heart diseases are 2 to 5 times more common among middle-aged men than women.[34] In a study done by the World Health Organization, sex contributes to approximately 40% of the variation in sex ratios of coronary heart disease mortality.[40] Another study reports similar results finding that sex differences explains nearly half the risk associated with cardiovascular diseases[34] One of the proposed explanations for sex differences in cardiovascular diseases is hormonal difference.[34] Among women, estrogen is the predominant sex hormone. Estrogen may have protective effects on glucose metabolism and hemostatic system, and may have direct effect in improving endothelial cell function.[34] The production of estrogen decreases after menopause, and this may change the female lipid metabolism toward a more atherogenic form by decreasing the HDL cholesterol level while increasing LDL and total cholesterol levels.[34]
Among men and women, there are differences in body weight, height, body fat distribution, heart rate, stroke volume, and arterial compliance.[35] In the very elderly, age-related large artery pulsatility and stiffness are more pronounced among women than men.[35] This may be caused by the women's smaller body size and arterial dimensions which are independent of menopause.[35]
Tobacco
Cigarettes are the major form of smoked tobacco.[3] Risks to health from tobacco use result not only from direct consumption of tobacco, but also from exposure to second-hand smoke.[3] Approximately 10% of cardiovascular disease is attributed to smoking;[3] however, people who quit smoking by age 30 have almost as low a risk of death as never smokers.[41]
Physical inactivity
Insufficient physical activity (defined as less than 5 x 30 minutes of moderate activity per week, or less than 3 x 20 minutes of vigorous activity per week) is currently the fourth leading risk factor for mortality worldwide.[3] In 2008, 31.3% of adults aged 15 or older (28.2% men and 34.4% women) were insufficiently physically active.[3] The risk of ischemic heart disease and diabetes mellitus is reduced by almost a third in adults who participate in 150 minutes of moderate physical activity each week (or equivalent).[42] In addition, physical activity assists weight loss and improves blood glucose control, blood pressure, lipid profile and insulin sensitivity. These effects may, at least in part, explain its cardiovascular benefits.[3]
Diet
High dietary intakes of saturated fat, trans-fats and salt, and low intake of fruits, vegetables and fish are linked to cardiovascular risk, although whether all these associations indicate causes is disputed. The World Health Organization attributes approximately 1.7 million deaths worldwide to low fruit and vegetable consumption.[3] Frequent consumption of high-energy foods, such as processed foods that are high in fats and sugars, promotes obesity and may increase cardiovascular risk.[3] The amount of dietary salt consumed may also be an important determinant of blood pressure levels and overall cardiovascular risk.[3] There is moderate quality evidence that reducing saturated fat intake for at least two years reduces the risk of cardiovascular disease.[43] High trans-fat intake has adverse effects on blood lipids and circulating inflammatory markers,[44] and elimination of trans-fat from diets has been widely advocated.[45][46] In 2018 the World Health Organization estimated that trans fats were the cause of more than half a million deaths per year.[46] There is evidence that higher consumption of sugar is associated with higher blood pressure and unfavorable blood lipids,[47] and sugar intake also increases the risk of diabetes mellitus.[48] High consumption of processed meats is associated with an increased risk of cardiovascular disease, possibly in part due to increased dietary salt intake.[20]
Alcohol
The relationship between alcohol consumption and cardiovascular disease is complex, and may depend on the amount of alcohol consumed.[49] There is a direct relationship between high levels of drinking alcohol and cardiovascular disease.[3] Drinking at low levels without episodes of heavy drinking may be associated with a reduced risk of cardiovascular disease,[50] but there is evidence that associations between moderate alcohol consumption and protection from stroke are non-causal.[51] At the population level, the health risks of drinking alcohol exceed any potential benefits.[3][52]
Celiac disease
Untreated celiac disease can cause the development of many types of cardiovascular diseases, most of which improve or resolve with a gluten-free diet and intestinal healing. However, delays in recognition and diagnosis of celiac disease can cause irreversible heart damage.[21]
Sleep
A lack of good sleep, in amount or quality, is documented as increasing cardiovascular risk in both adults and teens. Recommendations suggest that infants typically need 12 or more hours of sleep per day, adolescents at least eight or nine hours, and adults seven or eight. About one-third of adult Americans get less than the recommended seven hours of sleep per night, and in a study of teenagers, just 2.2 percent of those studied got enough sleep, many of whom did not get good quality sleep. Studies have shown that short sleepers getting less than seven hours sleep per night have a 10 percent to 30 percent higher risk of cardiovascular disease.[7][53]
Sleep disorders such as sleep-disordered breathing and insomnia, are also associated with a higher cardiometabolic risk.[54] An estimated 50 to 70 million Americans have insomnia, sleep apnea or other chronic sleep disorders.[citation needed]
In addition, sleep research displays differences in race and class. Short sleep and poor sleep tend to be more frequently reported in ethnic minorities than in whites. African-Americans report experiencing short durations of sleep five times more often than whites, possibly as a result of social and environmental factors. Black children and children living in disadvantaged neighborhoods have much higher rates of sleep apnea.[8]
Socioeconomic disadvantage
Cardiovascular disease has a greater impact on low- and middle-income countries compared to those with higher income.[55] Although data on the social patterns of cardiovascular disease in low- and middle-income countries is limited,[55] reports from high-income countries consistently demonstrate that low educational status or income are associated with a greater risk of cardiovascular disease.[56] Policies that have resulted in increased socio-economic inequalities have been associated with greater subsequent socio-economic differences in cardiovascular disease[55] implying a cause and effect relationship. Psychosocial factors, environmental exposures, health behaviours, and health-care access and quality contribute to socio-economic differentials in cardiovascular disease.[57] The Commission on Social Determinants of Health recommended that more equal distributions of power, wealth, education, housing, environmental factors, nutrition, and health care were needed to address inequalities in cardiovascular disease and non-communicable diseases.[58]
Air pollution
Particulate matter has been studied for its short- and long-term exposure effects on cardiovascular disease. Currently, airborne particles under 2.5 micrometers in diameter (PM2.5) are the major focus, in which gradients are used to determine CVD risk. Overall, long-term PM exposure increased rate of atherosclerosis and inflammation. In regards to short-term exposure (2 hours), every 25 μg/m3 of PM2.5 resulted in a 48% increase of CVD mortality risk.[59] In addition, after only 5 days of exposure, a rise in systolic (2.8 mmHg) and diastolic (2.7 mmHg) blood pressure occurred for every 10.5 μg/m3 of PM2.5.[59] Other research has implicated PM2.5 in irregular heart rhythm, reduced heart rate variability (decreased vagal tone), and most notably heart failure.[59][60] PM2.5 is also linked to carotid artery thickening and increased risk of acute myocardial infarction.[59][60]
Cardiovascular risk assessment
Existing cardiovascular disease or a previous cardiovascular event, such as a heart attack or stroke, is the strongest predictor of a future cardiovascular event.[61] Age, sex, smoking, blood pressure, blood lipids and diabetes are important predictors of future cardiovascular disease in people who are not known to have cardiovascular disease.[62] These measures, and sometimes others, may be combined into composite risk scores to estimate an individual's future risk of cardiovascular disease.[61] Numerous risk scores exist although their respective merits are debated.[63] Other diagnostic tests and biomarkers remain under evaluation but currently these lack clear-cut evidence to support their routine use. They include family history, coronary artery calcification score, high sensitivity C-reactive protein (hs-CRP), ankle–brachial pressure index, lipoprotein subclasses and particle concentration, lipoprotein(a), apolipoproteins A-I and B, fibrinogen, white blood cell count, homocysteine, N-terminal pro B-type natriuretic peptide (NT-proBNP), and markers of kidney function.[64][65] High blood phosphorus is also linked to an increased risk.[66]
Depression and traumatic stress
There is evidence that mental health problems, in particular depression and traumatic stress, is linked to cardiovascular diseases. Whereas mental health problems are known to be associated with risk factors for cardiovascular diseases such as smoking, poor diet, and a sedentary lifestyle, these factors alone do not explain the increased risk of cardiovascular diseases seen in depression, stress, and anxiety.[67] Moreover, posttraumatic stress disorder is independently associated with increased risk for incident coronary heart disease, even after adjusting for depression and other covariates.[68]
Occupational exposure
Little is known about the relationship between work and cardiovascular disease, but links have been established between certain toxins, extreme heat and cold, exposure to tobacco smoke, and mental health concerns such as stress and depression.[69]
Non-chemical risk factors
A 2015 SBU-report looking at non-chemical factors found an association for those:[70]
- with mentally stressful work with a lack of control over their working situation — with an effort-reward imbalance[70]
- who experience low social support at work; who experience injustice or experience insufficient opportunities for personal development; or those who experience job insecurity[70]
- those who work night schedules; or have long working weeks[70]
- those who are exposed to noise[70]
Specifically the risk of stroke was also increased by exposure to ionizing radiation.[70] Hypertension develops more often in those who experience job strain and who have shift-work.[70] Differences between women and men in risk are small, however men risk having and dying of heart attacks or stroke twice as often as women during working life.[70]
Chemical risk factors
A 2017 SBU report found evidence that workplace exposure to silica dust, engine exhaust or welding fumes is associated with heart disease.[71] Associations also exist for exposure to arsenic, benzopyrenes, lead, dynamite, carbon disulphide, carbon monoxide, metalworking fluids and occupational exposure to tobacco smoke.[71] Working with the electrolytic production of aluminium or the production of paper when the sulphate pulping process is used is associated with heart disease.[71] An association was also found between heart disease and exposure to compounds which are no longer permitted in certain work environments, such as phenoxy acids containing TCDD(dioxin) or asbestos.[71]
Workplace exposure to silica dust or asbestos is also associated with pulmonary heart disease. There is evidence that workplace exposure to lead, carbon disulphide, phenoxyacids containing TCDD, as well as working in an environment where aluminum is being electrolytically produced, is associated with stroke.[71]
Somatic mutations
As of 2017, evidence suggests that certain leukemia-associated mutations in blood cells may also lead to increased risk of cardiovascular disease. Several large-scale research projects looking at human genetic data have found a robust link between the presence of these mutations, a condition known as clonal hematopoiesis, and cardiovascular disease-related incidents and mortality.[72]
Radiation therapy
Radiation treatments (RT) for cancer can increase the risk of heart disease and death, as observed in breast cancer therapy.[73] Therapeutic radiation increases the risk of a subsequent heart attack or stroke by 1.5 to 4 times;[74] the increase depends on the dose strength, volume, and location. Use of concomitant chemotherapy, e.g. anthracyclines, is an aggravating risk factor.[75] The occurrence rate of RT induced cardiovascular disease is estimated between 10% and 30%.[75]
Side-effects from radiation therapy for cardiovascular diseases have been termed radiation-induced heart disease or radiation-induced cardiovascular disease.[76][77] Symptoms are dose-dependent and include cardiomyopathy, myocardial fibrosis, valvular heart disease, coronary artery disease, heart arrhythmia and peripheral artery disease. Radiation-induced fibrosis, vascular cell damage and oxidative stress can lead to these and other late side-effect symptoms.[76]
Pathophysiology

Population-based studies show that atherosclerosis, the major precursor of cardiovascular disease, begins in childhood. The Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study demonstrated that intimal lesions appear in all the aortas and more than half of the right coronary arteries of youths aged 7–9 years.[79]
Obesity and diabetes mellitus are linked to cardiovascular disease,[80] as are a history of chronic kidney disease and hypercholesterolaemia.[81] In fact, cardiovascular disease is the most life-threatening of the diabetic complications and diabetics are two- to four-fold more likely to die of cardiovascular-related causes than nondiabetics.[82][83][84]
Screening
Screening ECGs (either at rest or with exercise) are not recommended in those without symptoms who are at low risk.[85] This includes those who are young without risk factors.[86] In those at higher risk the evidence for screening with ECGs is inconclusive.[87] Additionally echocardiography, myocardial perfusion imaging, and cardiac stress testing is not recommended in those at low risk who do not have symptoms.[88] Some biomarkers may add to conventional cardiovascular risk factors in predicting the risk of future cardiovascular disease; however, the value of some biomarkers is questionable.[89][90] Ankle-brachial index (ABI), high-sensitivity C-reactive protein (hsCRP), and coronary artery calcium, are also of unclear benefit in those without symptoms as of 2018.[91]
The NIH recommends lipid testing in children beginning at the age of 2 if there is a family history of heart disease or lipid problems.[92] It is hoped that early testing will improve lifestyle factors in those at risk such as diet and exercise.[93]
Screening and selection for primary prevention interventions has traditionally been done through absolute risk using a variety of scores (ex. Framingham or Reynolds risk scores).[94] This stratification has separated people who receive the lifestyle interventions (generally lower and intermediate risk) from the medication (higher risk). The number and variety of risk scores available for use has multiplied, but their efficacy according to a 2016 review was unclear due to lack of external validation or impact analysis.[95] Risk stratification models often lack sensitivity for population groups and do not account for the large number of negative events among the intermediate and low risk groups.[94] As a result, future preventative screening appears to shift toward applying prevention according to randomized trial results of each intervention rather than large-scale risk assessment.
Prevention
Up to 90% of cardiovascular disease may be preventable if established risk factors are avoided.[9][96] Currently practised measures to prevent cardiovascular disease include:
- Maintaining a healthy diet, such as the Mediterranean diet, a vegetarian, vegan or another plant-based diet.[97][98][99][100]
- Replacing saturated fat with healthier choices: Clinical trials show that replacing saturated fat with polyunsaturated vegetable oil reduced CVD by 30%. Prospective observational studies show that in many populations lower intake of saturated fat coupled with higher intake of polyunsaturated and monounsaturated fat is associated with lower rates of CVD.[101]
- Decrease body fat if overweight or obese.[102] The effect of weight loss is often difficult to distinguish from dietary change, and evidence on weight reducing diets is limited.[103] In observational studies of people with severe obesity, weight loss following bariatric surgery is associated with a 46% reduction in cardiovascular risk.[104]
- Limit alcohol consumption to the recommended daily limits.[97] People who moderately consume alcoholic drinks have a 25–30% lower risk of cardiovascular disease.[105][106] However, people who are genetically predisposed to consume less alcohol have lower rates of cardiovascular disease[107] suggesting that alcohol itself may not be protective. Excessive alcohol intake increases the risk of cardiovascular disease[108][106] and consumption of alcohol is associated with increased risk of a cardiovascular event in the day following consumption.[106]
- Decrease non-HDL cholesterol.[109][110] Statin treatment reduces cardiovascular mortality by about 31%.[111]
- Stopping smoking and avoidance of second-hand smoke.[97] Stopping smoking reduces risk by about 35%.[112]
- At least 150 minutes (2 hours and 30 minutes) of moderate exercise per week.[113][114]
- Lower blood pressure, if elevated. A 10 mmHg reduction in blood pressure reduces risk by about 20%.[115] Lowering blood pressure appears to be effective even at normal blood pressure ranges.[116][117][118]
- Decrease psychosocial stress.[119] This measure may be complicated by imprecise definitions of what constitute psychosocial interventions.[120] Mental stress–induced myocardial ischemia is associated with an increased risk of heart problems in those with previous heart disease.[121] Severe emotional and physical stress leads to a form of heart dysfunction known as Takotsubo syndrome in some people.[122] Stress, however, plays a relatively minor role in hypertension.[123] Specific relaxation therapies are of unclear benefit.[124][125]
- Not enough sleep also raises the risk of high blood pressure. Adults need about 7–9 hours of sleep. Sleep apnea is also a major risk as it causes breathing to stop briefly, which can put stress on the body which can raise the risk of heart disease.[126][127]
Most guidelines recommend combining preventive strategies. There is some evidence that interventions aiming to reduce more than one cardiovascular risk factor may have beneficial effects on blood pressure, body mass index and waist circumference; however, evidence was limited and the authors were unable to draw firm conclusions on the effects on cardiovascular events and mortality.[128]
There is additional evidence to suggest that providing people with a cardiovascular disease risk score may reduce risk factors by a small amount compared to usual care.[129] However, there was some uncertainty as to whether providing these scores had any effect on cardiovascular disease events. It is unclear whether or not dental care in those with periodontitis affects their risk of cardiovascular disease.[130] According to a 2021 WHO study, working 55+ hours a week raises the risk of stroke by 35% and the risk of dying from heart conditions by 17%, when compared to a 35-40 hours week.[131]
Diet
A diet high in fruits and vegetables decreases the risk of cardiovascular disease and death.[132]
A 2021 review found that plant-based diets can provide a risk reduction for CVD if a healthy plant-based diet is consumed. Unhealthy plant-based diets do not provide benefits over diets including meat.[98] A similar meta-analysis and systematic review also looked into dietary patterns and found "that diets lower in animal foods and unhealthy plant foods, and higher in healthy plant foods are beneficial for CVD prevention".[99] A 2018 meta-analysis of observational studies concluded that "In most countries, a vegan diet is associated with a more favourable cardio-metabolic profile compared to an omnivorous diet."[100]
Evidence suggests that the Mediterranean diet may improve cardiovascular outcomes.[133] There is also evidence that a Mediterranean diet may be more effective than a low-fat diet in bringing about long-term changes to cardiovascular risk factors (e.g., lower cholesterol level and blood pressure).[134]
The DASH diet (high in nuts, fish, fruits and vegetables, and low in sweets, red meat and fat) has been shown to reduce blood pressure,[135] lower total and low density lipoprotein cholesterol[136] and improve metabolic syndrome;[137] but the long-term benefits have been questioned.[138] A high-fiber diet is associated with lower risks of cardiovascular disease.[139]
Worldwide, dietary guidelines recommend a reduction in saturated fat,[140] and although the role of dietary fat in cardiovascular disease is complex and controversial there is a long-standing consensus that replacing saturated fat with unsaturated fat in the diet is sound medical advice.[141] Total fat intake has not been found to be associated with cardiovascular risk.[142][143] A 2020 systematic review found moderate quality evidence that reducing saturated fat intake for at least 2 years caused a reduction in cardiovascular events.[144] A 2015 meta-analysis of observational studies however did not find a convincing association between saturated fat intake and cardiovascular disease.[145] Variation in what is used as a substitute for saturated fat may explain some differences in findings.[141] The benefit from replacement with polyunsaturated fats appears greatest,[146] while replacement of saturated fats with carbohydrates does not appear to have a beneficial effect.[146] A diet high in trans fatty acids is associated with higher rates of cardiovascular disease,[147] and in 2015 the Food and Drug Administration (FDA) determined that there was 'no longer a consensus among qualified experts that partially hydrogenated oils (PHOs), which are the primary dietary source of industrially produced trans fatty acids (IP-TFA), are generally recognized as safe (GRAS) for any use in human food'.[148] There is conflicting evidence concerning whether dietary supplements of omega-3 fatty acids (a type of polyunsaturated essential fatty acid) added to diet improve cardiovascular risk.[149][150]
The benefits of recommending a low-salt diet in people with high or normal blood pressure are not clear.[151] In those with heart failure, after one study was left out, the rest of the trials show a trend to benefit.[152][153] Another review of dietary salt concluded that there is strong evidence that high dietary salt intake increases blood pressure and worsens hypertension, and that it increases the number of cardiovascular disease events; both as a result of the increased blood pressure and probably through other mechanisms.[154][155] Moderate evidence was found that high salt intake increases cardiovascular mortality; and some evidence was found for an increase in overall mortality, strokes, and left ventricular hypertrophy.[154]
Intermittent fasting
Overall, the current body of scientific evidence is uncertain on whether intermittent fasting could prevent cardiovascular disease.[156] Intermittent fasting may help people lose more weight than regular eating patterns, but was not different from energy restriction diets.[156]
Medication
Blood pressure medication reduces cardiovascular disease in people at risk,[115] irrespective of age,[157] the baseline level of cardiovascular risk,[158] or baseline blood pressure.[159] The commonly-used drug regimens have similar efficacy in reducing the risk of all major cardiovascular events, although there may be differences between drugs in their ability to prevent specific outcomes.[160] Larger reductions in blood pressure produce larger reductions in risk,[160] and most people with high blood pressure require more than one drug to achieve adequate reduction in blood pressure.[161] Adherence to medications is often poor, and while mobile phone text messaging has been tried to improve adherence, there is insufficient evidence that it alters secondary prevention of cardiovascular disease.[162]
Statins are effective in preventing further cardiovascular disease in people with a history of cardiovascular disease.[163] As the event rate is higher in men than in women, the decrease in events is more easily seen in men than women.[163] In those at risk, but without a history of cardiovascular disease (primary prevention), statins decrease the risk of death and combined fatal and non-fatal cardiovascular disease.[164] The benefit, however, is small.[165] A United States guideline recommends statins in those who have a 12% or greater risk of cardiovascular disease over the next ten years.[166] Niacin, fibrates and CETP Inhibitors, while they may increase HDL cholesterol do not affect the risk of cardiovascular disease in those who are already on statins.[167] Fibrates lower the risk of cardiovascular and coronary events, but there is no evidence to suggest that they reduce all-cause mortality.[168]
Anti-diabetic medication may reduce cardiovascular risk in people with Type 2 diabetes, although evidence is not conclusive.[169] A meta-analysis in 2009 including 27,049 participants and 2,370 major vascular events showed a 15% relative risk reduction in cardiovascular disease with more-intensive glucose lowering over an average follow-up period of 4.4 years, but an increased risk of major hypoglycemia.[170]
Aspirin has been found to be of only modest benefit in those at low risk of heart disease, as the risk of serious bleeding is almost equal to the protection against cardiovascular problems.[171] In those at very low risk, including those over the age of 70, it is not recommended.[172][173] The United States Preventive Services Task Force recommends against use of aspirin for prevention in women less than 55 and men less than 45 years old; however, it is recommended for some older people.[174]
The use of vasoactive agents for people with pulmonary hypertension with left heart disease or hypoxemic lung diseases may cause harm and unnecessary expense.[175]
Antibiotics for secondary prevention of coronary heart disease
Antibiotics may help patients with coronary disease to reduce the risk of heart attacks and strokes.[176] However, evidence in 2021 suggests that antibiotics for secondary prevention of coronary heart disease are harmful, with increased mortality and occurrence of stroke;[176] the use of antibiotics is not supported for preventing secondary coronary heart disease.
Physical activity
Exercise-based cardiac rehabilitation following a heart attack reduces the risk of death from cardiovascular disease and leads to less hospitalizations.[177] There have been few high-quality studies of the benefits of exercise training in people with increased cardiovascular risk but no history of cardiovascular disease.[178]
A systematic review estimated that inactivity is responsible for 6% of the burden of disease from coronary heart disease worldwide.[179] The authors estimated that 121,000 deaths from coronary heart disease could have been averted in Europe in 2008 if people had not been physically inactive. Low-quality evidence from a limited number of studies suggest that yoga has beneficial effects on blood pressure and cholesterol.[180] Tentative evidence suggests that home-based exercise programs may be more efficient at improving exercise adherence.[181]
Dietary supplements
While a healthy diet is beneficial, the effect of antioxidant supplementation (vitamin E, vitamin C, etc.) or vitamins has not been shown to protect against cardiovascular disease and in some cases may possibly result in harm.[182][183][184][185] Mineral supplements have also not been found to be useful.[186] Niacin, a type of vitamin B3, may be an exception with a modest decrease in the risk of cardiovascular events in those at high risk.[187][188] Magnesium supplementation lowers high blood pressure in a dose-dependent manner.[189] Magnesium therapy is recommended for people with ventricular arrhythmia associated with torsades de pointes who present with long QT syndrome, and for the treatment of people with digoxin intoxication-induced arrhythmias.[190] There is no evidence that omega-3 fatty acid supplementation is beneficial.[191] A 2022 review found that some dietary supplements, including micronutrients, may reduce risk factors for cardiovascular disease.[192]
Management
Cardiovascular disease is treatable with initial treatment primarily focused on diet and lifestyle interventions.[3] Influenza may make heart attacks and strokes more likely and therefore influenza vaccination may decrease the chance of cardiovascular events and death in people with heart disease.[193]
Proper CVD management necessitates a focus on MI and stroke cases due to their combined high mortality rate, keeping in mind the cost-effectiveness of any intervention, especially in developing countries with low or middle-income levels.[94] Regarding MI, strategies using aspirin, atenolol, streptokinase or tissue plasminogen activator have been compared for quality-adjusted life-year (QALY) in regions of low and middle income. The costs for a single QALY for aspirin and atenolol were less than US$25, streptokinase was about $680, and t-PA was $16,000.[194] Aspirin, ACE inhibitors, beta-blockers, and statins used together for secondary CVD prevention in the same regions showed single QALY costs of $350.[194]
There are also surgical or procedural interventions that can save someone's life or prolong it. For heart valve problems, a person could have surgery to replace the valve. For arrhythmias, a pacemaker can be put in place to help reduce abnormal heart rhythms and for a heart attack, there are multiple options two of these are a coronary angioplasty and a coronary artery bypass surgery.[195]
There is probably no additional benefit in terms of mortality and serious adverse events when blood pressure targets were lowered to ≤ 135/85 mmHg from ≤ 140 to 160/90 to 100 mmHg.[196]
Epidemiology
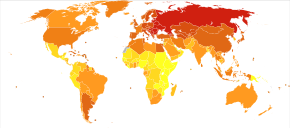
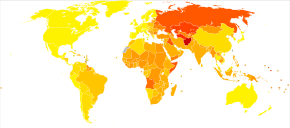
Cardiovascular diseases are the leading cause of death worldwide and in all regions except Africa.[3] In 2008, 30% of all global death was attributed to cardiovascular diseases. Death caused by cardiovascular diseases are also higher in low- and middle-income countries as over 80% of all global deaths caused by cardiovascular diseases occurred in those countries. It is also estimated that by 2030, over 23 million people will die from cardiovascular diseases each year.
It is estimated that 60% of the world's cardiovascular disease burden will occur in the South Asian subcontinent despite only accounting for 20% of the world's population. This may be secondary to a combination of genetic predisposition and environmental factors. Organizations such as the Indian Heart Association are working with the World Heart Federation to raise awareness about this issue.[197]
Research
There is evidence that cardiovascular disease existed in pre-history,[198] and research into cardiovascular disease dates from at least the 18th century.[199] The causes, prevention, and/or treatment of all forms of cardiovascular disease remain active fields of biomedical research, with hundreds of scientific studies being published on a weekly basis.
Recent areas of research include the link between inflammation and atherosclerosis[200] the potential for novel therapeutic interventions,[201] and the genetics of coronary heart disease.[202]
References
- ^ "Heart disease". Mayo Clinic. 2022-08-25.
- ^ a b Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. (January 2013). "Heart disease and stroke statistics--2013 update: a report from the American Heart Association". Circulation. 127 (1): e6–e245. doi:10.1161/cir.0b013e31828124ad. PMC 5408511. PMID 23239837.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad Shanthi M, Pekka P, Norrving B (2011). Global Atlas on Cardiovascular Disease Prevention and Control (PDF). World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. pp. 3–18. ISBN 978-92-4-156437-3. Archived (PDF) from the original on 2014-08-17.
- ^ a b c Naghavi M, Wang H, Lozano R, Davis A, Liang X, Zhou M, et al. (GBD 2013 Mortality and Causes of Death Collaborators) (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ^ a b Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ^ Petersen KS, Kris-Etherton PM (2021-11-28). "Diet quality assessment and the relationship between diet quality and cardiovascular disease risk". Nutrients. 13 (12): 4305. doi:10.3390/nu13124305. ISSN 2072-6643. PMC 8706326. PMID 34959857.
- ^ a b Jackson CL, Redline S, Emmons KM (March 2015). "Sleep as a potential fundamental contributor to disparities in cardiovascular health". Annual Review of Public Health. 36 (1): 417–40. doi:10.1146/annurev-publhealth-031914-122838. PMC 4736723. PMID 25785893.
- ^ a b Wang R, Dong Y, Weng J, Kontos EZ, Chervin RD, Rosen CL, et al. (January 2017). "Associations among Neighborhood, Race, and Sleep Apnea Severity in Children. A Six-City Analysis". Annals of the American Thoracic Society. 14 (1): 76–84. doi:10.1513/AnnalsATS.201609-662OC. PMC 5291481. PMID 27768852.
- ^ a b McGill HC, McMahan CA, Gidding SS (March 2008). "Preventing heart disease in the 21st century: implications of the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study". Circulation. 117 (9): 1216–27. doi:10.1161/CIRCULATIONAHA.107.717033. PMID 18316498.
- ^ O'Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, et al. (August 2016). "Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study". Lancet. 388 (10046): 761–75. doi:10.1016/S0140-6736(16)30506-2. PMID 27431356. S2CID 39752176.
- ^ Spinks A, Glasziou PP, Del Mar CB (2021-12-09). "Antibiotics for treatment of sore throat in children and adults". The Cochrane Database of Systematic Reviews. 2021 (12): CD000023. doi:10.1002/14651858.CD000023.pub5. ISSN 1469-493X. PMC 8655103. PMID 34881426.
- ^ Sutcliffe P, Connock M, Gurung T, Freeman K, Johnson S, Ngianga-Bakwin K, et al. (2013). "Aspirin in primary prevention of cardiovascular disease and cancer: a systematic review of the balance of evidence from reviews of randomized trials". PLOS ONE. 8 (12): e81970. Bibcode:2013PLoSO...881970S. doi:10.1371/journal.pone.0081970. PMC 3855368. PMID 24339983.
- ^ Sutcliffe P, Connock M, Gurung T, Freeman K, Johnson S, Kandala NB, et al. (September 2013). "Aspirin for prophylactic use in the primary prevention of cardiovascular disease and cancer: a systematic review and overview of reviews". Health Technology Assessment. 17 (43): 1–253. doi:10.3310/hta17430. PMC 4781046. PMID 24074752.
- ^ a b Institute of Medicine of the National Academies (2010). "Epidemiology of Cardiovascular Disease". In Fuster V, Kelly BB (eds.). Promoting cardiovascular health in the developing world : a critical challenge to achieve global health. Washington, DC: National Academies Press. ISBN 978-0-309-14774-3. Archived from the original on 2017-09-08.
- ^ Moran AE, Forouzanfar MH, Roth GA, Mensah GA, Ezzati M, Murray CJ, et al. (April 2014). "Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: the Global Burden of Disease 2010 study". Circulation. 129 (14): 1483–92. doi:10.1161/circulationaha.113.004042. PMC 4181359. PMID 24573352.
- ^ a b "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 2009-11-11.
- ^ "Vascular Diseases: MedlinePlus". www.nlm.nih.gov. Retrieved 2015-06-23.
- ^ Fuster V, Kelly BB, eds. (2010). Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. Washington, DC: National Academies Press. ISBN 978-0-309-14774-3.
- ^ Finks SW, Airee A, Chow SL, Macaulay TE, Moranville MP, Rogers KC, et al. (April 2012). "Key articles of dietary interventions that influence cardiovascular mortality". Pharmacotherapy. 32 (4): e54-87. doi:10.1002/j.1875-9114.2011.01087.x. PMID 22392596. S2CID 36437057.
- ^ a b Micha R, Michas G, Mozaffarian D (December 2012). "Unprocessed red and processed meats and risk of coronary artery disease and type 2 diabetes--an updated review of the evidence". Current Atherosclerosis Reports. 14 (6): 515–24. doi:10.1007/s11883-012-0282-8. PMC 3483430. PMID 23001745.
- ^ a b Ciaccio EJ, Lewis SK, Biviano AB, Iyer V, Garan H, Green PH (August 2017). "Cardiovascular involvement in celiac disease". World Journal of Cardiology (Review). 9 (8): 652–666. doi:10.4330/wjc.v9.i8.652. PMC 5583538. PMID 28932354.
- ^ Duell PB, Welty FK, Miller M, Chait A, Hammond G, Ahmad Z, et al. (April 2022). "Nonalcoholic Fatty Liver Disease and Cardiovascular Risk: A Scientific Statement From the American Heart Association". Arteriosclerosis, Thrombosis, and Vascular Biology. 42 (6): e168–e185. doi:10.1161/ATV.0000000000000153. PMID 35418240. S2CID 248155592.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. (2004). "Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study". Lancet. 364 (9438): 937–52. doi:10.1016/S0140-6736(04)17018-9. hdl:10983/21615. PMID 15364185. S2CID 30811593.
- ^ McPhee S (2012). Current medical diagnosis & treatment. New York: McGraw-Hill Medical. pp. 430. ISBN 978-0-07-176372-1.
- ^ Eckel RH (November 1997). "Obesity and heart disease: a statement for healthcare professionals from the Nutrition Committee, American Heart Association". Circulation. 96 (9): 3248–50. doi:10.1161/01.CIR.96.9.3248. PMID 9386201.
- ^ Kathiresan S, Srivastava D (March 2012). "Genetics of human cardiovascular disease". Cell. 148 (6): 1242–57. doi:10.1016/j.cell.2012.03.001. PMC 3319439. PMID 22424232.
- ^ a b Semsarian C, Ingles J, Ross SB, Dunwoodie SL, Bagnall RD, Kovacic JC (2021-05-25). "Precision Medicine in Cardiovascular Disease: Genetics and Impact on Phenotypes: JACC Focus Seminar 1/5". Journal of the American College of Cardiology. 77 (20): 2517–2530. doi:10.1016/j.jacc.2020.12.071. ISSN 0735-1097. PMID 34016265. S2CID 235073575.
- ^ Nikpay M, Goel A, Won HH, Hall LM, Willenborg C, Kanoni S, et al. (October 2015). "A comprehensive 1,000 Genomes-based genome-wide association meta-analysis of coronary artery disease" (PDF). Nature Genetics. 47 (10): 1121–1130. doi:10.1038/ng.3396. PMC 4589895. PMID 26343387 – via University of Dundee.
- ^ MacRae CA, Vasan RS (June 2016). "The Future of Genetics and Genomics: Closing the Phenotype Gap in Precision Medicine". Circulation. 133 (25): 2634–9. doi:10.1161/CIRCULATIONAHA.116.022547. PMC 6188655. PMID 27324359.
- ^ a b c Finegold JA, Asaria P, Francis DP (September 2013). "Mortality from ischaemic heart disease by country, region, and age: statistics from World Health Organisation and United Nations". International Journal of Cardiology. 168 (2): 934–45. doi:10.1016/j.ijcard.2012.10.046. PMC 3819990. PMID 23218570.
- ^ D'Adamo E, Guardamagna O, Chiarelli F, Bartuli A, Liccardo D, Ferrari F, et al. (2015). "Atherogenic dyslipidemia and cardiovascular risk factors in obese children". International Journal of Endocrinology. 2015: 912047. doi:10.1155/2015/912047. PMC 4309297. PMID 25663838.
- ^ "Understand Your Risk of Heart Attack". American Heart Association.http://www.heart.org/HEARTORG/Conditions/HeartAttack/UnderstandYourRiskofHeartAttack/Understand-Your-Risk-of-Heart-Attack_UCM_002040_Article.jsp
- ^ Mackay J, Mensah G, Mendis S, Greenland K (January 2004). The Atlas of Heart Disease and Stroke. World Health Organization and U. S. Centers for Disease Control and Prevention. hdl:10665/43007. ISBN 978-92-4-156276-8.
- ^ a b c d e f g Jousilahti P, Vartiainen E, Tuomilehto J, Puska P (March 1999). "Sex, age, cardiovascular risk factors, and coronary heart disease: a prospective follow-up study of 14 786 middle-aged men and women in Finland". Circulation. 99 (9): 1165–72. doi:10.1161/01.cir.99.9.1165. PMID 10069784.
- ^ a b c d Jani B, Rajkumar C (June 2006). "Ageing and vascular ageing". Postgraduate Medical Journal. 82 (968): 357–62. doi:10.1136/pgmj.2005.036053. PMC 2563742. PMID 16754702.
- ^ a b "Cardiovascular disease risk factors". World Heart Federation. 2012. Archived from the original on 2012-05-10.
- ^ "Diabetes raises women's risk of heart disease more than for men". NPR.org. May 22, 2014. Archived from the original on May 23, 2014. Retrieved May 23, 2014.
- ^ "Pregnancy complications increase the risk of heart attacks and stroke in women with high blood pressure". NIHR Evidence (Plain English summary). National Institute for Health and Care Research. 2023-11-21. doi:10.3310/nihrevidence_60660. S2CID 265356623.
- ^ Al Khalaf S, Chappell LC, Khashan AS, McCarthy FP, O'Reilly ÉJ (July 2023). "Association Between Chronic Hypertension and the Risk of 12 Cardiovascular Diseases Among Parous Women: The Role of Adverse Pregnancy Outcomes". Hypertension. 80 (7): 1427–1438. doi:10.1161/HYPERTENSIONAHA.122.20628. PMID 37170819.
- ^ Jackson R, Chambles L, Higgins M, Kuulasmaa K, Wijnberg L, Williams D (WHO MONICA Project, and ARIC Study.) Sex difference in ischaemic heart disease mortality and risk factors in 46 communities: an ecologic analysis. Cardiovasc Risk Factors. 1999; 7:43–54.
- ^ Doll R, Peto R, Boreham J, Sutherland I (June 2004). "Mortality in relation to smoking: 50 years' observations on male British doctors". BMJ. 328 (7455): 1519. doi:10.1136/bmj.38142.554479.AE. PMC 437139. PMID 15213107.
- ^ World Health Organization, UNAIDS (2007). Prevention of Cardiovascular Disease. World Health Organization. pp. 3–. ISBN 978-92-4-154726-0. Archived from the original on 27 April 2016.
- ^ Hooper L, Martin N, Jimoh OF, Kirk C, Foster E, Abdelhamid AS (August 2020). "Reduction in saturated fat intake for cardiovascular disease". The Cochrane Database of Systematic Reviews. 2020 (8): CD011737. doi:10.1002/14651858.CD011737.pub3. PMC 8092457. PMID 32827219.
- ^ Booker CS, Mann JI (July 2008). "Trans fatty acids and cardiovascular health: translation of the evidence base". Nutrition, Metabolism, and Cardiovascular Diseases. 18 (6): 448–56. doi:10.1016/j.numecd.2008.02.005. PMID 18468872.
- ^ Remig V, Franklin B, Margolis S, Kostas G, Nece T, Street JC (April 2010). "Trans fats in America: a review of their use, consumption, health implications, and regulation". Journal of the American Dietetic Association. 110 (4): 585–92. doi:10.1016/j.jada.2009.12.024. hdl:2097/6377. PMID 20338284.
- ^ a b "WHO plan to eliminate industrially-produced trans-fatty acids from global food supply" (Press release). World Health Organization. 14 May 2018.
- ^ Te Morenga LA, Howatson AJ, Jones RM, Mann J (July 2014). "Dietary sugars and cardiometabolic risk: systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids". The American Journal of Clinical Nutrition. 100 (1): 65–79. doi:10.3945/ajcn.113.081521. PMID 24808490.
- ^ Howard BV, Wylie-Rosett, J (Jul 23, 2002). "Sugar and cardiovascular disease: A statement for healthcare professionals from the Committee on Nutrition of the Council on Nutrition, Physical Activity, and Metabolism of the American Heart Association". Circulation. 106 (4): 523–7. doi:10.1161/01.cir.0000019552.77778.04. PMID 12135957. S2CID 1589727.
- ^ Bell S, Daskalopoulou M, Rapsomaniki E, George J, Britton A, Bobak M, et al. (March 2017). "Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: population based cohort study using linked health records". BMJ. 356: j909. doi:10.1136/bmj.j909. PMC 5594422. PMID 28331015.
- ^ Mukamal KJ, Chen CM, Rao SR, Breslow RA (March 2010). "Alcohol consumption and cardiovascular mortality among U.S. adults, 1987 to 2002". Journal of the American College of Cardiology. 55 (13): 1328–35. doi:10.1016/j.jacc.2009.10.056. PMC 3865979. PMID 20338493.
- ^ Millwood IY, Walters RG, Mei XW, Guo Y, Yang L, Bian Z, et al. (May 2019). "Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500 000 men and women in China". Lancet. 393 (10183): 1831–1842. doi:10.1016/S0140-6736(18)31772-0. PMC 6497989. PMID 30955975.
- ^ World Health Organization (2011). Global Status Report on Alcohol and Health. World Health Organization. ISBN 978-92-4-156415-1. Archived from the original on 2016-05-07.
- ^ Cespedes Feliciano EM, Quante M, Rifas-Shiman SL, Redline S, Oken E, Taveras EM (July 2018). "Objective Sleep Characteristics and Cardiometabolic Health in Young Adolescents". Pediatrics. 142 (1): e20174085. doi:10.1542/peds.2017-4085. PMC 6260972. PMID 29907703. Retrieved 28 June 2021.
- ^ St-Onge MP, Grandner MA, Brown D, Conroy MB, Jean-Louis G, Coons M, et al. (November 2016). "Sleep Duration and Quality: Impact on Lifestyle Behaviors and Cardiometabolic Health: A Scientific Statement From the American Heart Association". Circulation (Review). 134 (18): e367–e386. doi:10.1161/CIR.0000000000000444. PMC 5567876. PMID 27647451.
- ^ a b c Di Cesare M, Khang YH, Asaria P, Blakely T, Cowan MJ, Farzadfar F, et al. (February 2013). "Inequalities in non-communicable diseases and effective responses". Lancet. 381 (9866): 585–97. doi:10.1016/S0140-6736(12)61851-0. hdl:10906/80012. PMID 23410608. S2CID 41892834.
- ^ Mackenbach JP, Cavelaars AE, Kunst AE, Groenhof F (July 2000). "Socioeconomic inequalities in cardiovascular disease mortality; an international study". European Heart Journal. 21 (14): 1141–51. doi:10.1053/euhj.1999.1990. PMID 10924297. S2CID 8747779.
- ^ Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A (November 2009). "Socioeconomic status and cardiovascular disease: risks and implications for care". Nature Reviews. Cardiology. 6 (11): 712–22. doi:10.1038/nrcardio.2009.163. PMID 19770848. S2CID 21835944.
- ^ World Health Organization (2008). Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health : Commission on Social Determinants of Health Final Report. World Health Organization. pp. 26–. ISBN 978-92-4-156370-3. Archived from the original on 2016-05-01.
- ^ a b c d Franchini M, Mannucci PM (March 2012). "Air pollution and cardiovascular disease". Thrombosis Research. 129 (3): 230–4. doi:10.1016/j.thromres.2011.10.030. PMID 22113148.
- ^ a b Sun Q, Hong X, Wold LE (June 2010). "Cardiovascular effects of ambient particulate air pollution exposure". Circulation. 121 (25): 2755–65. doi:10.1161/CIRCULATIONAHA.109.893461. PMC 2924678. PMID 20585020.
- ^ a b Tunstall-Pedoe H (March 2011). "Cardiovascular Risk and Risk Scores: ASSIGN, Framingham, QRISK and others: how to choose". Heart. 97 (6): 442–4. doi:10.1136/hrt.2010.214858. PMID 21339319. S2CID 6420111.
- ^ World Health Organization (2007). Prevention of Cardiovascular Disease: Guidelines for Assessment and Management of Cardiovascular Risk. World Health Organization. ISBN 978-92-4-154717-8. Archived from the original on 2016-05-06.
- ^ van Staa TP, Gulliford M, Ng ES, Goldacre B, Smeeth L (2014). "Prediction of cardiovascular risk using Framingham, ASSIGN and QRISK2: how well do they predict individual rather than population risk?". PLOS ONE. 9 (10): e106455. Bibcode:2014PLoSO...9j6455V. doi:10.1371/journal.pone.0106455. PMC 4182667. PMID 25271417.

- ^ Hlatky MA, Greenland P, Arnett DK, Ballantyne CM, Criqui MH, Elkind MS, et al. (May 2009). "Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association". Circulation. 119 (17): 2408–16. doi:10.1161/CIRCULATIONAHA.109.192278. PMC 2956982. PMID 19364974.
- ^ Eckel RH, Cornier MA (August 2014). "Update on the NCEP ATP-III emerging cardiometabolic risk factors". BMC Medicine. 12 (1): 115. doi:10.1186/1741-7015-12-115. PMC 4283079. PMID 25154373.

- ^ Bai W, Li J, Liu J (October 2016). "Serum phosphorus, cardiovascular and all-cause mortality in the general population: A meta-analysis". Clinica Chimica Acta; International Journal of Clinical Chemistry. 461: 76–82. doi:10.1016/j.cca.2016.07.020. PMID 27475981.
- ^ Cohen BE, Edmondson D, Kronish IM (November 2015). "State of the Art Review: Depression, Stress, Anxiety, and Cardiovascular Disease". American Journal of Hypertension. 28 (11): 1295–302. doi:10.1093/ajh/hpv047. PMC 4612342. PMID 25911639.
- ^ Edmondson D, Kronish IM, Shaffer JA, Falzon L, Burg MM (November 2013). "Posttraumatic stress disorder and risk for coronary heart disease: a meta-analytic review". American Heart Journal. 166 (5): 806–14. doi:10.1016/j.ahj.2013.07.031. PMC 3815706. PMID 24176435.
- ^ "NIOSH Program Portfolio : Cancer, Reproductive, and Cardiovascular Diseases : Program Description". CDC. Archived from the original on 2016-05-15. Retrieved 2016-06-07.
- ^ a b c d e f g h Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU) (2015-08-26). "Occupational Exposures and Cardiovascular Disease". www.sbu.se. Archived from the original on 2017-06-14. Retrieved 2017-06-01.
- ^ a b c d e Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU). "Occupational health and safety – chemical exposure". www.sbu.se. Archived from the original on 2017-06-06. Retrieved 2017-06-01.
- ^ Jan M, Ebert BL, Jaiswal S (January 2017). "Clonal hematopoiesis". Seminars in Hematology. 54 (1): 43–50. doi:10.1053/j.seminhematol.2016.10.002. PMC 8045769. PMID 28088988.
- ^ Taylor CW, Nisbet A, McGale P, Darby SC (December 2007). "Cardiac exposures in breast cancer radiotherapy: 1950s-1990s". International Journal of Radiation Oncology, Biology, Physics. 69 (5): 1484–95. doi:10.1016/j.ijrobp.2007.05.034. PMID 18035211.
- ^ Weintraub NL, Jones WK, Manka D (March 2010). "Understanding radiation-induced vascular disease". Journal of the American College of Cardiology. 55 (12): 1237–1239. doi:10.1016/j.jacc.2009.11.053. PMC 3807611. PMID 20298931.
- ^ a b Benveniste MF, Gomez D, Carter BW, Betancourt Cuellar SL, Shroff GS, Benveniste AP, et al. (March 7, 2019). "Recognizing Radiation Therapy–related Complications in the Chest". RadioGraphics. 39 (2): 353. doi:10.1148/rg.2019180061. PMID 30844346. S2CID 73477338. Retrieved 24 August 2023.
- ^ a b Klee NS, McCarthy CG, Martinez-Quinones P, Webb RC (November 2017). "Out of the frying pan and into the fire: damage-associated molecular patterns and cardiovascular toxicity following cancer therapy". Therapeutic Advances in Cardiovascular Disease. 11 (11): 297–317. doi:10.1177/1753944717729141. PMC 5933669. PMID 28911261.
- ^ Belzile-Dugas E, Eisenberg MJ (September 2021). "Radiation-Induced Cardiovascular Disease: Review of an Underrecognized Pathology". J Am Heart Assoc. 10 (18): e021686. doi:10.1161/JAHA.121.021686. PMC 8649542. PMID 34482706.
- ^ Bertazzo S, Gentleman E, Cloyd KL, Chester AH, Yacoub MH, Stevens MM (June 2013). "Nano-analytical electron microscopy reveals fundamental insights into human cardiovascular tissue calcification". Nature Materials. 12 (6): 576–83. Bibcode:2013NatMa..12..576B. doi:10.1038/nmat3627. PMC 5833942. PMID 23603848.
- ^ Vanhecke TE, Miller WM, Franklin BA, Weber JE, McCullough PA (October 2006). "Awareness, knowledge, and perception of heart disease among adolescents". European Journal of Cardiovascular Prevention and Rehabilitation. 13 (5): 718–23. doi:10.1097/01.hjr.0000214611.91490.5e. PMID 17001210. S2CID 36312234.
- ^ Highlander P, Shaw GP (February 2010). "Current pharmacotherapeutic concepts for the treatment of cardiovascular disease in diabetics". Therapeutic Advances in Cardiovascular Disease. 4 (1): 43–54. doi:10.1177/1753944709354305. PMID 19965897. S2CID 23913203.
- ^ NPS Medicinewise (1 March 2011). "NPS Prescribing Practice Review 53: Managing lipids". Archived from the original on 19 March 2011. Retrieved 1 August 2011.
- ^ Kvan E, Pettersen KI, Sandvik L, Reikvam A (October 2007). "High mortality in diabetic patients with acute myocardial infarction: cardiovascular co-morbidities contribute most to the high risk". International Journal of Cardiology. 121 (2): 184–8. doi:10.1016/j.ijcard.2006.11.003. PMID 17184858.
- ^ Norhammar A, Malmberg K, Diderholm E, Lagerqvist B, Lindahl B, Rydén L, et al. (February 2004). "Diabetes mellitus: the major risk factor in unstable coronary artery disease even after consideration of the extent of coronary artery disease and benefits of revascularization". Journal of the American College of Cardiology. 43 (4): 585–91. doi:10.1016/j.jacc.2003.08.050. PMID 14975468.
- ^ DECODE, European Diabetes Epidemiology Group (August 1999). "Glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria. The DECODE study group. European Diabetes Epidemiology Group. Diabetes Epidemiology: Collaborative analysis Of Diagnostic criteria in Europe". Lancet. 354 (9179): 617–21. doi:10.1016/S0140-6736(98)12131-1. PMID 10466661. S2CID 54227479.
- ^ Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. (June 2018). "Screening for Cardiovascular Disease Risk With Electrocardiography: US Preventive Services Task Force Recommendation Statement". JAMA. 319 (22): 2308–2314. doi:10.1001/jama.2018.6848. PMID 29896632.
- ^ Maron BJ, Friedman RA, Kligfield P, Levine BD, Viskin S, Chaitman BR, et al. (October 2014). "Assessment of the 12-lead ECG as a screening test for detection of cardiovascular disease in healthy general populations of young people (12-25 Years of Age): a scientific statement from the American Heart Association and the American College of Cardiology". Circulation. 130 (15): 1303–34. doi:10.1161/CIR.0000000000000025. PMID 25223981.
- ^ Moyer VA (October 2012). "Screening for coronary heart disease with electrocardiography: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 157 (7): 512–8. doi:10.7326/0003-4819-157-7-201210020-00514. PMID 22847227.
- ^ Chou R (March 2015). "Cardiac screening with electrocardiography, stress echocardiography, or myocardial perfusion imaging: advice for high-value care from the American College of Physicians". Annals of Internal Medicine. 162 (6): 438–47. doi:10.7326/M14-1225. PMID 25775317. S2CID 207538193.
- ^ Wang TJ, Gona P, Larson MG, Tofler GH, Levy D, Newton-Cheh C, et al. (December 2006). "Multiple biomarkers for the prediction of first major cardiovascular events and death". The New England Journal of Medicine. 355 (25): 2631–9. doi:10.1056/NEJMoa055373. PMID 17182988. S2CID 196411135.
- ^ Spence JD (November 2006). "Technology Insight: ultrasound measurement of carotid plaque--patient management, genetic research, and therapy evaluation". Nature Clinical Practice. Neurology. 2 (11): 611–9. doi:10.1038/ncpneuro0324. PMID 17057748. S2CID 26077254.
- ^ Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. (July 2018). "Risk Assessment for Cardiovascular Disease With Nontraditional Risk Factors: US Preventive Services Task Force Recommendation Statement". JAMA. 320 (3): 272–280. doi:10.1001/jama.2018.8359. PMID 29998297.
- ^ Expert Panel on Integrated Guidelines for Cardiovascular Health Risk Reduction in Children Adolescents (December 2011). "Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report". Pediatrics. 128 (Supplement 5): S213-56. doi:10.1542/peds.2009-2107C. PMC 4536582. PMID 22084329.
- ^ Saenger AK (August 2012). "Universal lipid screening in children and adolescents: a baby step toward primordial prevention?". Clinical Chemistry. 58 (8): 1179–81. doi:10.1373/clinchem.2012.182287. PMID 22510399.
- ^ a b c Mann DL, Zipes DP, Libby P, Bonow RO, Braunwald E (2014). Braunwald's heart disease : a textbook of cardiovascular medicine (Tenth ed.). Philadelphia. ISBN 978-1-4557-5133-4. OCLC 890409638.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Damen JA, Hooft L, Schuit E, Debray TP, Collins GS, Tzoulaki I, et al. (May 2016). "Prediction models for cardiovascular disease risk in the general population: systematic review". BMJ. 353: i2416. doi:10.1136/bmj.i2416. PMC 4868251. PMID 27184143.
- ^ McNeal CJ, Dajani T, Wilson D, Cassidy-Bushrow AE, Dickerson JB, Ory M (January 2010). "Hypercholesterolemia in youth: opportunities and obstacles to prevent premature atherosclerotic cardiovascular disease". Current Atherosclerosis Reports. 12 (1): 20–8. doi:10.1007/s11883-009-0072-0. PMID 20425267. S2CID 37833889.
- ^ a b c "Heart Attack—Prevention". NHS Direct. 28 November 2019.
- ^ a b Quek J, Lim G, Lim WH, Ng CH, So WZ, Toh J, et al. (2021-11-05). "The Association of Plant-Based Diet With Cardiovascular Disease and Mortality: A Meta-Analysis and Systematic Review of Prospect Cohort Studies". Frontiers in Cardiovascular Medicine. 8: 756810. doi:10.3389/fcvm.2021.756810. ISSN 2297-055X. PMC 8604150. PMID 34805312.
- ^ a b Gan ZH, Cheong HC, Tu YK, Kuo PH (2021-11-05). "Association between Plant-Based Dietary Patterns and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Cohort Studies". Nutrients. 13 (11): 3952. doi:10.3390/nu13113952. ISSN 2072-6643. PMC 8624676. PMID 34836208.
- ^ a b Benatar JR, Stewart RA (2018). "Cardiometabolic risk factors in vegans; A meta-analysis of observational studies". PLOS ONE. 13 (12): e0209086. Bibcode:2018PLoSO..1309086B. doi:10.1371/journal.pone.0209086. ISSN 1932-6203. PMC 6301673. PMID 30571724.
- ^ Frank M. Sacks, Alice H. Lichtenstein, Jason H.Y. Wu, Lawrence J. Appel, Mark A. Creager, Penny M. Kris-Etherton, Michael Miller, Eric B. Rimm, Lawrence L. Rudel, Jennifer G. Robinson, Neil J. Stone, and Linda V. Van Horn: Dietary Fats and Cardiovascular Disease: A Presidential Advisory From the American Heart Association, 15 Jun 2017, https://doi.org/10.1161/CIR.0000000000000510Circulation 2017;136:e1–e23, https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000510
- ^ McTigue KM, Hess R, Ziouras J (September 2006). "Obesity in older adults: a systematic review of the evidence for diagnosis and treatment". Obesity. 14 (9): 1485–97. doi:10.1038/oby.2006.171. PMID 17030958. S2CID 45241607.
- ^ Semlitsch T, Krenn C, Jeitler K, Berghold A, Horvath K, Siebenhofer A (February 2021). "Long-term effects of weight-reducing diets in people with hypertension". The Cochrane Database of Systematic Reviews. 2021 (2): CD008274. doi:10.1002/14651858.CD008274.pub4. PMC 8093137. PMID 33555049.
- ^ Kwok CS, Pradhan A, Khan MA, Anderson SG, Keavney BD, Myint PK, et al. (April 2014). "Bariatric surgery and its impact on cardiovascular disease and mortality: a systematic review and meta-analysis". International Journal of Cardiology. 173 (1): 20–8. doi:10.1016/j.ijcard.2014.02.026. hdl:2164/3181. PMID 24636546.
- ^ Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA (February 2011). "Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis". BMJ. 342: d671. doi:10.1136/bmj.d671. PMC 3043109. PMID 21343207.
- ^ a b c Mostofsky E, Chahal HS, Mukamal KJ, Rimm EB, Mittleman MA (March 2016). "Alcohol and Immediate Risk of Cardiovascular Events: A Systematic Review and Dose-Response Meta-Analysis". Circulation. 133 (10): 979–87. doi:10.1161/CIRCULATIONAHA.115.019743. PMC 4783255. PMID 26936862.
- ^ Holmes MV, Dale CE, Zuccolo L, Silverwood RJ, Guo Y, Ye Z, et al. (July 2014). "Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data". BMJ. 349: g4164. doi:10.1136/bmj.g4164. PMC 4091648. PMID 25011450.
- ^ Klatsky AL (May 2009). "Alcohol and cardiovascular diseases". Expert Review of Cardiovascular Therapy. 7 (5): 499–506. doi:10.1586/erc.09.22. PMID 19419257. S2CID 23782870.
- ^ McMahan CA, Gidding SS, Malcom GT, Tracy RE, Strong JP, McGill HC (October 2006). "Pathobiological determinants of atherosclerosis in youth risk scores are associated with early and advanced atherosclerosis". Pediatrics. 118 (4): 1447–55. doi:10.1542/peds.2006-0970. PMID 17015535. S2CID 37741456.
- ^ Raitakari OT, Rönnemaa T, Järvisalo MJ, Kaitosaari T, Volanen I, Kallio K, et al. (December 2005). "Endothelial function in healthy 11-year-old children after dietary intervention with onset in infancy: the Special Turku Coronary Risk Factor Intervention Project for children (STRIP)". Circulation. 112 (24): 3786–94. doi:10.1161/CIRCULATIONAHA.105.583195. PMID 16330680.
- ^ Chou R, Dana T, Blazina I, Daeges M, Jeanne TL (November 2016). "Statins for Prevention of Cardiovascular Disease in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force". JAMA. 316 (19): 2008–2024. doi:10.1001/jama.2015.15629. PMID 27838722.
- ^ Critchley J, Capewell S (2004-01-01). Critchley JA (ed.). "Smoking cessation for the secondary prevention of coronary heart disease". The Cochrane Database of Systematic Reviews (1): CD003041. doi:10.1002/14651858.CD003041.pub2. PMID 14974003. (Retracted, see doi:10.1002/14651858.CD003041.pub3, PMID 22336785)
- ^ "Chapter 4: Active Adults". health.gov. Archived from the original on 2017-03-13.
- ^ "Physical activity guidelines for adults". NHS Choices. 2018-04-26. Archived from the original on 2017-02-19.
- ^ a b Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. (March 2016). "Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis". Lancet. 387 (10022): 957–967. doi:10.1016/S0140-6736(15)01225-8. PMID 26724178.
- ^ "Many more people could benefit from blood pressure-lowering medication". medicalxpress.com. Retrieved 14 June 2021.
- ^ "expert reaction to study looking at pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure | Science Media Centre". Retrieved 14 June 2021.
- ^ Adler A, Agodoa L, Algra A, Asselbergs FW, Beckett NS, Berge E, et al. (May 2021). "Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis". Lancet. 397 (10285): 1625–1636. doi:10.1016/S0140-6736(21)00590-0. PMC 8102467. PMID 33933205.
 Available under CC BY 4.0.
Available under CC BY 4.0.
- ^ Linden W, Stossel C, Maurice J (April 1996). "Psychosocial interventions for patients with coronary artery disease: a meta-analysis". Archives of Internal Medicine. 156 (7): 745–52. doi:10.1001/archinte.1996.00440070065008. PMID 8615707. S2CID 45312858.
- ^ Thompson DR, Ski CF (December 2013). "Psychosocial interventions in cardiovascular disease--what are they?" (PDF). European Journal of Preventive Cardiology. 20 (6): 916–7. doi:10.1177/2047487313494031. PMID 24169589. S2CID 35497445.
- ^ Wei J, Rooks C, Ramadan R, Shah AJ, Bremner JD, Quyyumi AA, et al. (July 2014). "Meta-analysis of mental stress-induced myocardial ischemia and subsequent cardiac events in patients with coronary artery disease". The American Journal of Cardiology. 114 (2): 187–92. doi:10.1016/j.amjcard.2014.04.022. PMC 4126399. PMID 24856319.
- ^ Pelliccia F, Greco C, Vitale C, Rosano G, Gaudio C, Kaski JC (August 2014). "Takotsubo syndrome (stress cardiomyopathy): an intriguing clinical condition in search of its identity". The American Journal of Medicine. 127 (8): 699–704. doi:10.1016/j.amjmed.2014.04.004. hdl:11573/562721. PMID 24754972.
- ^ Marshall IJ, Wolfe CD, McKevitt C (July 2012). "Lay perspectives on hypertension and drug adherence: systematic review of qualitative research". BMJ. 345: e3953. doi:10.1136/bmj.e3953. PMC 3392078. PMID 22777025.
- ^ Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. (February 2006). "Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials". Journal of Hypertension. 24 (2): 215–33. doi:10.1097/01.hjh.0000199800.72563.26. PMID 16508562. S2CID 9125890.
- ^ Abbott RA, Whear R, Rodgers LR, Bethel A, Thompson Coon J, Kuyken W, et al. (May 2014). "Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: A systematic review and meta-analysis of randomised controlled trials". Journal of Psychosomatic Research. 76 (5): 341–51. doi:10.1016/j.jpsychores.2014.02.012. hdl:10871/19935. PMID 24745774.
- ^ U.S. National Library of Medicine. (2021, March 24). Heart Disease Prevention. MedlinePlus. https://medlineplus.gov/howtopreventheartdisease.html.
- ^ U.S. Department of Health and Human Services. (n.d.). Cardiovascular Disease. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/cardiovascular-disease.
- ^ Uthman OA, Hartley L, Rees K, Taylor F, Ebrahim S, Clarke A (August 2015). "Multiple risk factor interventions for primary prevention of cardiovascular disease in low- and middle-income countries" (PDF). The Cochrane Database of Systematic Reviews. 2015 (8): CD011163. doi:10.1002/14651858.CD011163.pub2. PMC 6999125. PMID 26272648.
- ^ Karmali KN, Persell SD, Perel P, Lloyd-Jones DM, Berendsen MA, Huffman MD (March 2017). "Risk scoring for the primary prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews. 3 (6): CD006887. doi:10.1002/14651858.CD006887.pub4. PMC 6464686. PMID 28290160.
- ^ Ye Z, Cao Y, Miao C, Liu W, Dong L, Lv Z, et al. (2022-10-04). "Periodontal therapy for primary or secondary prevention of cardiovascular disease in people with periodontitis". The Cochrane Database of Systematic Reviews. 2022 (10): CD009197. doi:10.1002/14651858.CD009197.pub5. ISSN 1469-493X. PMC 9531722. PMID 36194420.
- ^ Pega F, Náfrádi B, Momen NC, Ujita Y, Streicher KN, Prüss-Üstün AM, et al. (2021-09-01). "Global, regional, and national burdens of ischemic heart disease and stroke attributable to exposure to long working hours for 194 countries, 2000–2016: A systematic analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury". Environment International. 154: 106595. Bibcode:2021EnInt.15406595P. doi:10.1016/j.envint.2021.106595. ISSN 0160-4120. PMC 8204267. PMID 34011457.
- ^ Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, et al. (July 2014). "Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies". BMJ. 349: g4490. doi:10.1136/bmj.g4490. PMC 4115152. PMID 25073782.
- ^ Walker C, Reamy BV (April 2009). "Diets for cardiovascular disease prevention: what is the evidence?". American Family Physician. 79 (7): 571–8. PMID 19378874.
- ^ Nordmann AJ, Suter-Zimmermann K, Bucher HC, Shai I, Tuttle KR, Estruch R, et al. (September 2011). "Meta-analysis comparing Mediterranean to low-fat diets for modification of cardiovascular risk factors". The American Journal of Medicine. 124 (9): 841–51.e2. doi:10.1016/j.amjmed.2011.04.024. PMID 21854893. Archived from the original on 2013-12-20.
- ^ Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. (January 2001). "Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group". The New England Journal of Medicine. 344 (1): 3–10. doi:10.1056/NEJM200101043440101. PMID 11136953.
- ^ Obarzanek E, Sacks FM, Vollmer WM, Bray GA, Miller ER, Lin PH, et al. (July 2001). "Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hypertension (DASH) Trial". The American Journal of Clinical Nutrition. 74 (1): 80–9. doi:10.1093/ajcn/74.1.80. PMID 11451721.
- ^ Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi T, Azizi F (December 2005). "Beneficial effects of a Dietary Approaches to Stop Hypertension eating plan on features of the metabolic syndrome". Diabetes Care. 28 (12): 2823–31. doi:10.2337/diacare.28.12.2823. PMID 16306540.
- ^ Logan AG (March 2007). "DASH Diet: time for a critical appraisal?". American Journal of Hypertension. 20 (3): 223–4. doi:10.1016/j.amjhyper.2006.10.006. PMID 17324730.
- ^ Hajishafiee M, Saneei P, Benisi-Kohansal S, Esmaillzadeh A (July 2016). "Cereal Fibre Intake and Risk of Mortality From All Causes, CVD, Cancer and Inflammatory Diseases: A Systematic Review and Meta-Analysis of Prospective Cohort Studies". The British Journal of Nutrition. 116 (2): 343–52. doi:10.1017/S0007114516001938. PMID 27193606.
- ^ Ramsden CE, Zamora D, Leelarthaepin B, Majchrzak-Hong SF, Faurot KR, Suchindran CM, et al. (February 2013). "Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis". BMJ. 346: e8707. doi:10.1136/bmj.e8707. PMC 4688426. PMID 23386268.
- ^ a b Lichtenstein AH (November 2019). "Dietary Fat and Cardiovascular Disease: Ebb and Flow Over the Last Half Century". Advances in Nutrition. 10 (Suppl_4): S332–S339. doi:10.1093/advances/nmz024. PMC 6855944. PMID 31728492.
- ^ Food and Agriculture Organization of the United Nations (2010). Fats and fatty acids in human nutrition: report of an expert consultation, 10-14 November 2008, Geneva. Rome: Food and Agriculture Organization of the United Nations. ISBN 978-92-5-106733-8. OCLC 712123395. Archived from the original on 2014-12-28.
- ^ Willett WC (July 2012). "Dietary fats and coronary heart disease". Journal of Internal Medicine. 272 (1): 13–24. doi:10.1111/j.1365-2796.2012.02553.x. PMID 22583051. S2CID 43493760.
- ^ Hooper L, Martin N, Jimoh OF, Kirk C, Foster E, Abdelhamid AS (21 August 2020). "Reduction in saturated fat intake for cardiovascular disease". The Cochrane Database of Systematic Reviews. 2020 (8): CD011737. doi:10.1002/14651858.CD011737.pub3. ISSN 1469-493X. PMC 8092457. PMID 32827219.
- ^ de Souza RJ, Mente A, Maroleanu A, Cozma AI, Ha V, Kishibe T, et al. (August 2015). "Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies". BMJ. 351 (h3978): h3978. doi:10.1136/bmj.h3978. PMC 4532752. PMID 26268692.
- ^ a b Sacks FM, Lichtenstein AH, Wu JH, Appel LJ, Creager MA, Kris-Etherton PM, et al. (July 2017). "Dietary Fats and Cardiovascular Disease: A Presidential Advisory From the American Heart Association". Circulation. 136 (3): e1–e23. doi:10.1161/CIR.0000000000000510. PMID 28620111. S2CID 367602.
- ^ Chowdhury R, Warnakula S, Kunutsor S, Crowe F, Ward HA, Johnson L, et al. (March 2014). "Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis". Annals of Internal Medicine. 160 (6): 398–406. doi:10.7326/M13-1788. PMID 24723079. S2CID 52013596.
- ^ Food Drug Administration H (May 2018). "Final Determination Regarding Partially Hydrogenated Oils. Notification; declaratory order; extension of compliance date". Federal Register. 83 (98): 23358–9. PMID 30019869.
- ^ Abdelhamid AS, Brown TJ, Brainard JS, Biswas P, Thorpe GC, Moore HJ, et al. (February 2020). "Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews. 2020 (3): CD003177. doi:10.1002/14651858.CD003177.pub5. PMC 7049091. PMID 32114706.
- ^ Aung T, Halsey J, Kromhout D, Gerstein HC, Marchioli R, Tavazzi L, et al. (March 2018). "Associations of Omega-3 Fatty Acid Supplement Use With Cardiovascular Disease Risks: Meta-analysis of 10 Trials Involving 77 917 Individuals". JAMA Cardiology. 3 (3): 225–234. doi:10.1001/jamacardio.2017.5205. PMC 5885893. PMID 29387889.
- ^ Adler AJ, Taylor F, Martin N, Gottlieb S, Taylor RS, Ebrahim S (December 2014). "Reduced dietary salt for the prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews. 2014 (12): CD009217. doi:10.1002/14651858.CD009217.pub3. PMC 6483405. PMID 25519688.
- ^ He FJ, MacGregor GA (July 2011). "Salt reduction lowers cardiovascular risk: meta-analysis of outcome trials" (PDF). Lancet. 378 (9789): 380–2. doi:10.1016/S0140-6736(11)61174-4. PMID 21803192. S2CID 43795786. Archived from the original (PDF) on 2013-12-20. Retrieved 2013-08-23.
- ^ Paterna S, Gaspare P, Fasullo S, Sarullo FM, Di Pasquale P (February 2008). "Normal-sodium diet compared with low-sodium diet in compensated congestive heart failure: is sodium an old enemy or a new friend?" (PDF). Clinical Science. 114 (3): 221–30. doi:10.1042/CS20070193. PMID 17688420. S2CID 2248777. (This paper currently has an expression of concern, see doi:10.1042/CS-20070193_EOC, PMID 32677681)
- ^ a b Bochud M, Marques-Vidal P, Burnier M, Paccaud F (2012). "Dietary Salt Intake and Cardiovascular Disease: Summarizing the Evidence". Public Health Reviews. 33 (2): 530–52. doi:10.1007/BF03391649. Archived from the original on 2013-12-21.
- ^ Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, et al. (April 2007). "Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP)". BMJ. 334 (7599): 885–8. doi:10.1136/bmj.39147.604896.55. PMC 1857760. PMID 17449506.
- ^ a b Allaf M, Elghazaly H, Mohamed OG, Fareen MF, Zaman S, Salmasi AM, et al. (Cochrane Heart Group) (January 2021). "Intermittent fasting for the prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews. 1 (3): CD013496. doi:10.1002/14651858.CD013496.pub2. PMC 8092432. PMID 33512717.
- ^ Turnbull F, Neal B, Ninomiya T, Algert C, Arima H, Barzi F, et al. (May 2008). "Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials". BMJ. 336 (7653): 1121–3. doi:10.1136/bmj.39548.738368.BE. PMC 2386598. PMID 18480116.
- ^ Blood Pressure Lowering Treatment Trialists' Collaboration (August 2014). "Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data". Lancet. 384 (9943): 591–598. doi:10.1016/S0140-6736(14)61212-5. PMID 25131978. S2CID 19951800.
- ^ Czernichow S, Zanchetti A, Turnbull F, Barzi F, Ninomiya T, Kengne AP, et al. (January 2011). "The effects of blood pressure reduction and of different blood pressure-lowering regimens on major cardiovascular events according to baseline blood pressure: meta-analysis of randomized trials". Journal of Hypertension. 29 (1): 4–16. doi:10.1097/HJH.0b013e32834000be. PMID 20881867. S2CID 10374187.
- ^ a b Turnbull F (November 2003). "Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials". Lancet (Submitted manuscript). 362 (9395): 1527–35. doi:10.1016/s0140-6736(03)14739-3. PMID 14615107. S2CID 10730075.
- ^ Go AS, Bauman MA, Coleman King SM, Fonarow GC, Lawrence W, Williams KA, et al. (April 2014). "An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention". Hypertension. 63 (4): 878–85. doi:10.1161/HYP.0000000000000003. PMC 10280688. PMID 24243703.
- ^ Redfern J, Tu Q, Hyun K, Hollings MA, Hafiz N, Zwack C, et al. (2024-03-27). "Mobile phone text messaging for medication adherence in secondary prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews. 2024 (3): CD011851. doi:10.1002/14651858.CD011851.pub3. ISSN 1469-493X. PMC 10966941. PMID 38533994.
- ^ a b Gutierrez J, Ramirez G, Rundek T, Sacco RL (June 2012). "Statin therapy in the prevention of recurrent cardiovascular events: a sex-based meta-analysis". Archives of Internal Medicine. 172 (12): 909–19. doi:10.1001/archinternmed.2012.2145. PMID 22732744.
- ^ Taylor F, Huffman MD, Macedo AF, Moore TH, Burke M, Davey Smith G, et al. (January 2013). "Statins for the primary prevention of cardiovascular disease" (PDF). The Cochrane Database of Systematic Reviews. 1 (1): CD004816. doi:10.1002/14651858.CD004816.pub5. PMC 6481400. PMID 23440795.
- ^ "Statins in primary cardiovascular prevention?". Prescrire International. 27 (195): 183. July–August 2018. Retrieved 4 August 2018.
- ^ Downs JR, O'Malley PG (August 2015). "Management of dyslipidemia for cardiovascular disease risk reduction: synopsis of the 2014 U.S. Department of Veterans Affairs and U.S. Department of Defense clinical practice guideline". Annals of Internal Medicine. 163 (4): 291–7. doi:10.7326/m15-0840. PMID 26099117.
- ^ Keene D, Price C, Shun-Shin MJ, Francis DP (July 2014). "Effect on cardiovascular risk of high density lipoprotein targeted drug treatments niacin, fibrates, and CETP inhibitors: meta-analysis of randomised controlled trials including 117,411 patients". BMJ. 349: g4379. doi:10.1136/bmj.g4379. PMC 4103514. PMID 25038074.
- ^ Jakob T, Nordmann AJ, Schandelmaier S, Ferreira-González I, Briel M, et al. (Cochrane Heart Group) (November 2016). "Fibrates for primary prevention of cardiovascular disease events". The Cochrane Database of Systematic Reviews. 11 (3): CD009753. doi:10.1002/14651858.CD009753.pub2. PMC 6464497. PMID 27849333.
- ^ Holman RR, Sourij H, Califf RM (June 2014). "Cardiovascular outcome trials of glucose-lowering drugs or strategies in type 2 diabetes". Lancet. 383 (9933): 2008–17. doi:10.1016/s0140-6736(14)60794-7. PMID 24910232. S2CID 5064731.
- ^ Turnbull FM, Abraira C, Anderson RJ, Byington RP, Chalmers JP, Duckworth WC, et al. (November 2009). "Intensive glucose control and macrovascular outcomes in type 2 diabetes". Diabetologia. 52 (11): 2288–98. doi:10.1007/s00125-009-1470-0. PMID 19655124.
- ^ Berger JS, Lala A, Krantz MJ, Baker GS, Hiatt WR (July 2011). "Aspirin for the prevention of cardiovascular events in patients without clinical cardiovascular disease: a meta-analysis of randomized trials". American Heart Journal. 162 (1): 115–24.e2. doi:10.1016/j.ahj.2011.04.006. PMID 21742097.
- ^ "Final Recommendation Statement Aspirin for the Prevention of Cardiovascular Disease: Preventive Medication". March 2009. Archived from the original on 10 January 2015. Retrieved 15 January 2015.
- ^ Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. (March 2019). "2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Journal of the American College of Cardiology. 74 (10): e177–e232. doi:10.1016/j.jacc.2019.03.010. PMC 7685565. PMID 30894318.
- ^ US Preventive Services Task Force (March 2009). "Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 150 (6): 396–404. doi:10.7326/0003-4819-150-6-200903170-00008. PMID 19293072.
- ^ American College of Chest Physicians, American Thoracic Society (September 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American College of Chest Physicians and American Thoracic Society, archived from the original on 3 November 2013, retrieved 6 January 2013
- ^ a b Sethi NJ, Safi S, Korang SK, Hróbjartsson A, Skoog M, Gluud C, et al. (Cochrane Heart Group) (February 2021). "Antibiotics for secondary prevention of coronary heart disease". The Cochrane Database of Systematic Reviews. 2 (5): CD003610. doi:10.1002/14651858.CD003610.pub4. PMC 8094925. PMID 33704780.
- ^ Dibben G, Faulkner J, Oldridge N, Rees K, Thompson DR, Zwisler AD, et al. (6 November 2021). "Exercise-based cardiac rehabilitation for coronary heart disease". The Cochrane Database of Systematic Reviews. 2021 (11): CD001800. doi:10.1002/14651858.CD001800.pub4. ISSN 1469-493X. PMC 8571912. PMID 34741536.
- ^ Seron P, Lanas F, Pardo Hernandez H, Bonfill Cosp X (August 2014). "Exercise for people with high cardiovascular risk". The Cochrane Database of Systematic Reviews. 2014 (8): CD009387. doi:10.1002/14651858.CD009387.pub2. PMC 6669260. PMID 25120097.
- ^ Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT (July 2012). "Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy". Lancet. 380 (9838): 219–29. doi:10.1016/S0140-6736(12)61031-9. PMC 3645500. PMID 22818936.
- ^ Hartley L, Dyakova M, Holmes J, Clarke A, Lee MS, Ernst E, et al. (May 2014). "Yoga for the primary prevention of cardiovascular disease" (PDF). The Cochrane Database of Systematic Reviews. 2014 (5): CD010072. doi:10.1002/14651858.CD010072.pub2. PMC 10075056. PMID 24825181.
- ^ Ashworth NL, Chad KE, Harrison EL, Reeder BA, Marshall SC (January 2005). "Home versus center based physical activity programs in older adults". The Cochrane Database of Systematic Reviews. 2005 (1): CD004017. doi:10.1002/14651858.cd004017.pub2. PMC 6464851. PMID 15674925.
- ^ Al-Khudairy L, Flowers N, Wheelhouse R, Ghannam O, Hartley L, Stranges S, et al. (March 2017). "Vitamin C supplementation for the primary prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews. 2017 (3): CD011114. doi:10.1002/14651858.CD011114.pub2. PMC 6464316. PMID 28301692.
- ^ Bhupathiraju SN, Tucker KL (August 2011). "Coronary heart disease prevention: nutrients, foods, and dietary patterns". Clinica Chimica Acta; International Journal of Clinical Chemistry. 412 (17–18): 1493–514. doi:10.1016/j.cca.2011.04.038. PMC 5945285. PMID 21575619.
- ^ Myung SK, Ju W, Cho B, Oh SW, Park SM, Koo BK, et al. (January 2013). "Efficacy of vitamin and antioxidant supplements in prevention of cardiovascular disease: systematic review and meta-analysis of randomised controlled trials". BMJ. 346: f10. doi:10.1136/bmj.f10. PMC 3548618. PMID 23335472.
- ^ Kim J, Choi J, Kwon SY, McEvoy JW, Blaha MJ, Blumenthal RS, et al. (July 2018). "Association of Multivitamin and Mineral Supplementation and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis". Circulation: Cardiovascular Quality and Outcomes. 11 (7): e004224. doi:10.1161/CIRCOUTCOMES.117.004224. PMID 29991644. S2CID 51615818.
- ^ Fortmann SP, Burda BU, Senger CA, Lin JS, Whitlock EP (December 2013). "Vitamin and mineral supplements in the primary prevention of cardiovascular disease and cancer: An updated systematic evidence review for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 159 (12): 824–34. doi:10.7326/0003-4819-159-12-201312170-00729. PMID 24217421.
- ^ Bruckert E, Labreuche J, Amarenco P (June 2010). "Meta-analysis of the effect of nicotinic acid alone or in combination on cardiovascular events and atherosclerosis". Atherosclerosis. 210 (2): 353–61. doi:10.1016/j.atherosclerosis.2009.12.023. PMID 20079494.
- ^ Lavigne PM, Karas RH (January 2013). "The current state of niacin in cardiovascular disease prevention: a systematic review and meta-regression". Journal of the American College of Cardiology. 61 (4): 440–446. doi:10.1016/j.jacc.2012.10.030. PMID 23265337.
- ^ Jee SH, Miller ER, Guallar E, Singh VK, Appel LJ, Klag MJ (August 2002). "The effect of magnesium supplementation on blood pressure: a meta-analysis of randomized clinical trials". American Journal of Hypertension. 15 (8): 691–6. doi:10.1016/S0895-7061(02)02964-3. PMID 12160191.
- ^ Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, et al. (September 2006). "ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society". Circulation. 114 (10): e385-484. doi:10.1161/CIRCULATIONAHA.106.178233. PMID 16935995.
- ^ Kwak SM, Myung SK, Lee YJ, Seo HG (May 2012). "Efficacy of omega-3 fatty acid supplements (eicosapentaenoic acid and docosahexaenoic acid) in the secondary prevention of cardiovascular disease: a meta-analysis of randomized, double-blind, placebo-controlled trials". Archives of Internal Medicine. 172 (9): 686–94. doi:10.1001/archinternmed.2012.262. PMID 22493407.
- ^ An P, Wan S, Luo Y, Luo J, Zhang X, Zhou S, et al. (13 December 2022). "Micronutrient supplementation to reduce cardiovascular risk". Journal of the American College of Cardiology. 80 (24): 2269–2285. doi:10.1016/j.jacc.2022.09.048. ISSN 0735-1097. PMID 36480969. S2CID 254343574.
- ^ Clar C, Oseni Z, Flowers N, Keshtkar-Jahromi M, Rees K (May 2015). "Influenza vaccines for preventing cardiovascular disease". The Cochrane Database of Systematic Reviews. 2015 (5): CD005050. doi:10.1002/14651858.CD005050.pub3. PMC 8511741. PMID 25940444. S2CID 205176857.
- ^ a b Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF (2018). Braunwald's Heart Disease E-Book: A Textbook of Cardiovascular Medicine. Elsevier Health Sciences. p. 15. ISBN 978-0-323-55593-7.
- ^ "What is Cardiovascular Disease?". www.heart.org. 31 May 2017.
- ^ Saiz LC, Gorricho J, Garjón J, Celaya C, Erviti J, Leache L (2022-11-18). "Blood pressure targets for the treatment of people with hypertension and cardiovascular disease". The Cochrane Database of Systematic Reviews. 2022 (11): CD010315. doi:10.1002/14651858.CD010315.pub5. ISSN 1469-493X. PMC 9673465. PMID 36398903.
- ^ Roo S. "Cardiac Disease Among South Asians: A Silent Epidemic". Indian Heart Association. Archived from the original on 2015-05-18. Retrieved 2018-12-31.
- ^ Thompson RC, Allam AH, Lombardi GP, Wann LS, Sutherland ML, Sutherland JD, et al. (April 2013). "Atherosclerosis across 4000 years of human history: the Horus study of four ancient populations". Lancet. 381 (9873): 1211–22. doi:10.1016/s0140-6736(13)60598-x. PMID 23489753. S2CID 16928278.
- ^ Alberti FB (2013-05-01). "John Hunter's Heart". The Bulletin of the Royal College of Surgeons of England. 95 (5): 168–69. doi:10.1308/003588413X13643054409261. ISSN 1473-6357.
- ^ Ruparelia N, Chai JT, Fisher EA, Choudhury RP (March 2017). "Inflammatory processes in cardiovascular disease: a route to targeted therapies". Nature Reviews. Cardiology. 14 (3): 133–144. doi:10.1038/nrcardio.2016.185. PMC 5525550. PMID 27905474.
- ^ Tang WH, Hazen SL (January 2017). "Atherosclerosis in 2016: Advances in new therapeutic targets for atherosclerosis". Nature Reviews. Cardiology. 14 (2): 71–72. doi:10.1038/nrcardio.2016.216. PMC 5880294. PMID 28094270.
- ^ Swerdlow DI, Humphries SE (February 2017). "Genetics of CHD in 2016: Common and rare genetic variants and risk of CHD". Nature Reviews. Cardiology. 14 (2): 73–74. doi:10.1038/nrcardio.2016.209. PMID 28054577. S2CID 13738641.
