Varicocele
| Varicocele | |
|---|---|
 | |
| Varicocele on the person's left testicle. Notice the swelling and slight enlargement of the left testicle, which is marked by an arrow. | |
| Pronunciation | |
| Specialty | Urology |
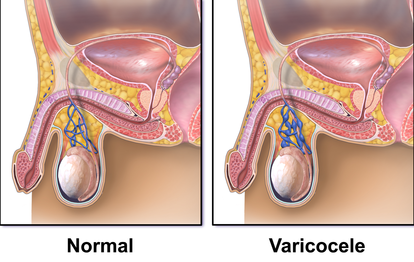
A varicocele is, in a man, an abnormal enlargement of the pampiniform venous plexus in the scrotum; in a woman, it is an abnormal painful swelling to the embryologically identical pampiniform venous plexus; it is more commonly called pelvic compression syndrome. In the male varicocele, this plexus of veins drains blood from the testicles back to the heart. The vessels originate in the abdomen and course down through the inguinal canal as part of the spermatic cord on their way to the testis. Varicoceles occur in around 15% to 20% of all men.[3][4] The incidence of varicocele increase with age.[citation needed]
Signs and symptoms
[edit]Varicocele might be noticed as soft lumps, usually above the testicle and mostly on the left side of the scrotum.[5] Right-sided and bilateral varicocele does also occur. Men with varicocele can feel symptoms of pain or heaviness in their scrotum.[5] Large varicoceles present as plexus of veins and may be described as a "bag of worms".[6][7] Varicocele is sometimes discovered when investigating the cause of male infertility.[8][9]
Cause
[edit]
There are three main theories as to the anatomical cause; the first has to do with the geometry of the veins, wherein the vein on the left side connects to the larger outflowing vein at a right angle, which tends to fail; the second is that testicular valves that are supposed to prevent backflow fail (venous insufficiency) leading to swelling and compression of the valveless pampiniform plexus; the third is due to excessive pressure in upstream veins, created by nutcracker syndrome.[10]
Pathophysiology
[edit]Often the greatest concern with respect to varicocele is its effect on male fertility. The relationship between varicocele and infertility is unclear. Some men with the condition are fertile, some have sperm that are normal in shape and move normally but are compromised in function, and some have sperm with abnormal shapes or that do not move well.[10] Theories as to how varicocele affects sperm function include damage via excess heat caused by the blood pooling and oxidative stress on sperm.[4][10][11][12]
Tobacco smoking and mutations in the gene expressing glutathione S-transferase Mu 1 both put men at risk for infertility; these factors may also exacerbate the risk that varicocele will affect fertility.[10]
Diagnosis
[edit]Following discovery of the sign of swelling comprising a mass, varicocele can be confirmed with scrotal ultrasound, which will show dilation of the vessels of the pampiniform plexus to be greater than 2.3 mm.[13]
-
Varicocele in ultrasound (left: testicle)
-
Varicocele
Criteria
[edit]A universally accepted system for categorizing varicoceles does not exist, but according to the classification criteria established in 1970 by Dubin and Amelar, most commonly varicoceles are clinically assessed and categorized into three grades as follows:[14][15]
- Grade 1 Varicocele: Characterized by the palpability of the varicocele only when the individual is in a standing position during the Valsalva maneuver.
- Grade 2 Varicocele: The varicocele is palpable not only during the Valsalva maneuver but also at rest while standing.
- Grade 3 Varicocele: The most severe grade, where the varicocele is not only palpable but also visible through the scrotal skin, without any additional maneuvers.
In the Sarteschi (1993) classification system, varicoceles are categorized into five grades:[16]
- Grade I: Reflux occurs solely at the groin level during the Valsalva maneuver, without evident scrotal deformation or testicular atrophy.
- Grade II: Reflux is limited to the proximal segment of the pampiniform plexus during the Valsalva maneuver, without scrotal deformation or testicular atrophy.
- Grade III: Reflux occurs in the distal vessels located at the lower scrotum exclusively during the Valsalva maneuver, and there is no scrotal deformation or testicular atrophy.
- Grade IV: Spontaneous reverse blood flow is present and intensifies during the Valsalva maneuver, resulting in scrotal deformation and the potential for testicular atrophy.
- Grade V: Resting reflux is evident within the dilated pampiniform plexus, possibly escalating during the Valsalva maneuver, and is consistently accompanied by testicular atrophy.
Imaging
[edit]Manual examination of scrotum is required for proper interpretation of ultrasound images. During ultrasound examination, diameters of veins in pampiniform plexus are measured and regurgitation is measured. The subject is then instructed to stand up and Valsalva maneuver is performed. The diameter is then measured and changes in blood flow direction is recorded to assess any regurgitation.[17]
Treatment
[edit]
The two most common surgical approaches are retroperitoneal (abdominal using laparoscopic surgery), infrainguinal/subinguinal (below the groin) and inguinal (groin using percutaneous embolization).[4] Possible complications of this procedure include hematoma (bleeding into tissues), hydrocele (accumulation of fluid around the affected testicle), infection, or injury to the scrotal tissue or structures. In addition, injury to the artery that supplies the testicle may occur, resulting in a loss of a testicle.[4]
Prognosis
[edit]Whether having varicocele surgery or embolization improves male fertility is controversial, as good clinical data is lacking.[9] There is tentative evidence that varicocelectomy may improve fertility in those with obvious findings and abnormal sperm;[4] however, this has a number needed to treat of 7 for varicocelectomy and 17 for embolization.[18][19] There are also studies showing that the regular surgery has no significant effect on infertility.[9] A 2012 Cochrane review (updated in 2021) found tentative but unclear evidence of improved fertility among males treated for varicocele.[20] Evidence for sclerotherapy is unclear as of 2015.[21]
Epidemiology
[edit]Around 15% to 20% of all adult males, up to 35% to 40% of men who are evaluated for male infertility, and around 80% of men who are infertile due to some other cause, have varicocele.[3][4][9]
External links
[edit]References
[edit]- ^ "Varicocele". Merriam-Webster.com Dictionary. Merriam-Webster. Retrieved 2016-01-21.
- ^ "Varicocele". Lexico UK English Dictionary. Oxford University Press. Archived from the original on 2020-12-04.
- ^ a b White, Wesley M.; Kim, Edward David; Mobley, Joe D (2 January 2019). "Varicocele: Epidemiology". Medscape. Retrieved 18 September 2019.
Although varicoceles appear in approximately 20% of the general male population, they are much more common in the subfertile population (40%).
- ^ a b c d e f Kupis, Ł; Dobroński, PA; Radziszewski, P (2015). "Varicocele as a source of male infertility - current treatment techniques". Central European Journal of Urology. 68 (3): 365–70. doi:10.5173/ceju.2015.642. PMC 4643713. PMID 26568883.
- ^ a b "Testicular lumps and swellings - Causes - NHS Choices". NHS Choices. 7 October 2014.
- ^ Cannarella, Rossella; Calogero, Aldo E.; Condorelli, Rosita A.; Giacone, Filippo; Aversa, Antonio; La Vignera, Sandro (8 September 2019). "Management and Treatment of Varicocele in Children and Adolescents: An Endocrinologic Perspective". Journal of Clinical Medicine. 9 (8): 1410. doi:10.3390/jcm8091410. PMC 6780349. PMID 31500355.
- ^ Leslie, Stephen W.; Sajjad, Hussain; Siref, Larry E. (7 October 2019). Varicocele. StatPearls [Internet]. PMID 28846314. Retrieved 20 January 2020.
- ^ "Low sperm count". NHS Choices. 2 August 2016.
- ^ a b c d Baazeem, Abdulaziz; Belzile, Eric; Ciampi, Antonio; Dohle, Gert; Jarvi, Keith; Salonia, Andrea; Weidner, Wolfgang; Zini, Armand (2011-10-01). "Varicocele and male factor infertility treatment: a new meta-analysis and review of the role of varicocele repair". European Urology. 60 (4): 796–808. doi:10.1016/j.eururo.2011.06.018. PMID 21733620.
- ^ a b c d Eisenberg, Michael L.; Lipshultz, Larry I. (2011-01-01). "Varicocele-induced infertility: Newer insights into its pathophysiology". Indian Journal of Urology. 27 (1): 58–64. doi:10.4103/0970-1591.78428. ISSN 0970-1591. PMC 3114589. PMID 21716891.
- ^ Hayden, Russell P.; Tanrikut, Cigdem (2016-05-01). "Testosterone and Varicocele". The Urologic Clinics of North America. 43 (2): 223–232. doi:10.1016/j.ucl.2016.01.009. ISSN 1558-318X. PMID 27132580.
- ^ Dabaja, Ali; Wosnitzer, Matthew; Goldstein, Marc (2013-08-01). "Varicocele and hypogonadism". Current Urology Reports. 14 (4): 309–314. doi:10.1007/s11934-013-0339-4. ISSN 1534-6285. PMID 23754533. S2CID 5477034.
- ^ Salam, MA (2013). Principles and Practice of Urology. New Delhi 110 002, India: Jaypee Brothers Medical Publishers. p. 752. ISBN 978-93-5025-260-4.
{{cite book}}: CS1 maint: location (link) - ^ Bertolotto, Michele; Cantisani, Vito; Drudi, Francesco Maria; Lotti, Francesco (September 2021). "Varicocoele. Classification and pitfalls". Andrology. 9 (5): 1322–1330. doi:10.1111/andr.13053. ISSN 2047-2919. PMC 8596817. PMID 34038625.
- ^ A. Hamada; et al. (2016). Varicocele and Male Infertility (PDF). SpringerBriefs in Reproductive Biology. doi:10.1007/978-3-319-24936-0. ISBN 978-3-319-24934-6. S2CID 5203944.
- ^ Namdev, Rupesh. "Varicocele grading on color Doppler | Radiology Reference Article | Radiopaedia.org". Radiopaedia. Retrieved 2023-10-04.
- ^ Lorenc T, Krupniewski L, Palczewski P, Gołębiowski M (December 2016). "The value of ultrasonography in the diagnosis of varicocele". Journal of Ultrasonography. 16 (67): 359–370. doi:10.15557/JoU.2016.0036. PMC 5269523. PMID 28138407.
- ^ Kroese, A. C. J.; Lange, N. M. de; Collins, J. A.; Evers, J. L. H. (2013-07-01). "Varicocele surgery, new evidence". Human Reproduction Update. 19 (4): 317. doi:10.1093/humupd/dmt004. PMID 23515200.
- ^ Li, Fuping; Yue, Huanxun; Yamaguchi, Kohei; Okada, Keisuke; Matsushita, Kei; Ando, Makoto; Chiba, Koji; Fujisawa, Masato (2012). "Effect of surgical repair on testosterone production in infertile men with varicocele: A meta-analysis". International Journal of Urology. 19 (2): 149–54. doi:10.1111/j.1442-2042.2011.02890.x. PMID 22059526. S2CID 20329833.
- ^ Persad, Emma; O'Loughlin, Clare Aa; Kaur, Simi; Wagner, Gernot; Matyas, Nina; Hassler-Di Fratta, Melanie Rosalia; Nussbaumer-Streit, Barbara (2021-04-23). "Surgical or radiological treatment for varicoceles in subfertile men". The Cochrane Database of Systematic Reviews. 2021 (4): CD000479. doi:10.1002/14651858.CD000479.pub6. ISSN 1469-493X. PMC 8408310. PMID 33890288.
- ^ Macleod, R; Biyani, CS; Cartledge, J; Eardley, I (13 July 2015). "Varicocele". BMJ Clinical Evidence. 2015. PMC 4500994. PMID 26168774.