Aspirin
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /əˌsiːtəlˌsælɪˈsɪlɪk/ |
| Trade names | Bayer Aspirin, others |
| Other names |
|
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682878 |
| License data | |
| Pregnancy category |
|
| Routes of administration | Oral, rectal |
| Drug class | Nonsteroidal anti-inflammatory drug (NSAID) |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 80–100%[6] |
| Protein binding | 80–90%[7] |
| Metabolism | Liver (CYP2C19 and possibly CYP3A), some is also hydrolysed to salicylate in the gut wall.[7] |
| Elimination half-life | Dose-dependent; 2–3 h for low doses (100 mg or less), 15–30 h for larger doses.[7] |
| Excretion | Urine (80–100%), sweat, saliva, feces[6] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.059 |
| Chemical and physical data | |
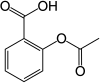
| Formula | C9H8O4 |
| Molar mass | 180.159 g·mol−1 |
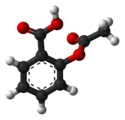
| 3D model (JSmol) | |
| Density | 1.40 g/cm3 |
| Melting point | 135 °C (275 °F) [9] |
| Boiling point | 140 °C (284 °F) (decomposes) |
| Solubility in water | 3 g/L |
| |
| |
| (verify) | |
Aspirin is the genericized trademark for acetylsalicylic acid (ASA), a nonsteroidal anti-inflammatory drug (NSAID) used to reduce pain, fever, and inflammation, and as an antithrombotic.[10] Specific inflammatory conditions that aspirin is used to treat include Kawasaki disease, pericarditis, and rheumatic fever.[10]
Aspirin is also used long-term to help prevent further heart attacks, ischaemic strokes, and blood clots in people at high risk.[10] For pain or fever, effects typically begin within 30 minutes.[10] Aspirin works similarly to other NSAIDs but also suppresses the normal functioning of platelets.[10]
One common adverse effect is an upset stomach.[10] More significant side effects include stomach ulcers, stomach bleeding, and worsening asthma.[10] Bleeding risk is greater among those who are older, drink alcohol, take other NSAIDs, or are on other blood thinners.[10] Aspirin is not recommended in the last part of pregnancy.[10] It is not generally recommended in children with infections because of the risk of Reye syndrome.[10] High doses may result in ringing in the ears.[10]
A precursor to aspirin found in the bark of the willow tree (genus Salix) has been used for its health effects for at least 2,400 years.[11][12] In 1853, chemist Charles Frédéric Gerhardt treated the medicine sodium salicylate with acetyl chloride to produce acetylsalicylic acid for the first time.[13] Over the next 50 years, other chemists, mostly of the German company Bayer, established the chemical structure and devised more efficient production methods.[13]: 69–75 Felix Hoffmann (or Arthur Eichengrün) of Bayer was the first to produce acetylsalicylic acid in a pure, stable form in 1897.[14] By 1899, Bayer had dubbed this drug Aspirin and was selling it globally.[15]: 27
Aspirin is available without medical prescription as a proprietary or generic medication[10] in most jurisdictions. It is one of the most widely used medications globally, with an estimated 40,000 tonnes (44,000 tons) (50 to 120 billion pills) consumed each year,[11][16] and is on the World Health Organization's List of Essential Medicines.[17] In 2022, it was the 36th most commonly prescribed medication in the United States, with more than 16 million prescriptions.[18][19]
Brand vs. generic name
[edit]In 1897, scientists at the Bayer company began studying acetylsalicylic acid as a less-irritating replacement medication for common salicylate medicines.[13]: 69–75 [20] By 1899, Bayer had named it "Aspirin" and was selling it around the world.[15]
Aspirin's popularity grew over the first half of the 20th century, leading to competition between many brands and formulations.[21] The word Aspirin was Bayer's brand name; however, its rights to the trademark were lost or sold in many countries.[21] The name is ultimately a blend of the prefix a(cetyl) + spir Spiraea, the meadowsweet plant genus from which the acetylsalicylic acid was originally derived at Bayer + -in, the common chemical suffix.[citation needed]
Chemical properties
[edit]Aspirin decomposes rapidly in solutions of ammonium acetate or the acetates, carbonates, citrates, or hydroxides of the alkali metals. It is stable in dry air, but gradually hydrolyses in contact with moisture to acetic and salicylic acids. In solution with alkalis, the hydrolysis proceeds rapidly and the clear solutions formed may consist entirely of acetate and salicylate.[22]
Like flour mills, factories producing aspirin tablets must control the amount of the powder that becomes airborne inside the building, because the powder-air mixture can be explosive. The National Institute for Occupational Safety and Health (NIOSH) has set a recommended exposure limit in the United States of 5 mg/m3 (time-weighted average).[23] In 1989, the Occupational Safety and Health Administration (OSHA) set a legal permissible exposure limit for aspirin of 5 mg/m3, but this was vacated by the AFL-CIO v. OSHA decision in 1993.[24]
Synthesis
[edit]The synthesis of aspirin is classified as an esterification reaction. Salicylic acid is treated with acetic anhydride, an acid derivative, causing a chemical reaction that turns salicylic acid's hydroxyl group into an ester group (R-OH → R-OCOCH3). This process yields aspirin and acetic acid, which is considered a byproduct of this reaction. Small amounts of sulfuric acid (and occasionally phosphoric acid) are almost always used as a catalyst. This method is commonly demonstrated in undergraduate teaching labs.[25]

Reaction between acetic acid and salicylic acid can also form aspirin but this esterification reaction is reversible and the presence of water can lead to hydrolysis of the aspirin. So, an anhydrous reagent is preferred.[26]
- Reaction mechanism
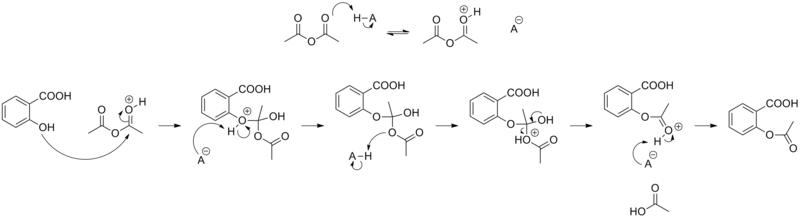
Formulations containing high concentrations of aspirin often smell like vinegar[27] because aspirin can decompose through hydrolysis in moist conditions, yielding salicylic and acetic acids.[28]
Physical properties
[edit]Aspirin, an acetyl derivative of salicylic acid, is a white, crystalline, weakly acidic substance that melts at 136 °C (277 °F),[9] and decomposes around 140 °C (284 °F).[29] Its acid dissociation constant (pKa) is 3.5 at 25 °C (77 °F).[30]
Polymorphism
[edit]Polymorphism, or the ability of a substance to form more than one crystal structure, is important in the development of pharmaceutical ingredients. Many drugs receive regulatory approval for only a single crystal form or polymorph.
Until 2005, there was only one proven polymorph of aspirin (Form I), though the existence of another polymorph was debated since the 1960s, and one report from 1981 reported that when crystallized in the presence of aspirin anhydride, the diffractogram of aspirin has weak additional peaks. Though at the time it was dismissed as mere impurity, it was, in retrospect, Form II aspirin.[31]
Form II was reported in 2005,[32][33] found after attempted co-crystallization of aspirin and levetiracetam from hot acetonitrile.
In form I, pairs of aspirin molecules form centrosymmetric dimers through the acetyl groups with the (acidic) methyl proton to carbonyl hydrogen bonds. In form II, each aspirin molecule forms the same hydrogen bonds, but with two neighbouring molecules instead of one. With respect to the hydrogen bonds formed by the carboxylic acid groups, both polymorphs form identical dimer structures. The aspirin polymorphs contain identical 2-dimensional sections and are therefore more precisely described as polytypes.[34]
Pure Form II aspirin could be prepared by seeding the batch with aspirin anhydrate in 15% weight.[31]
Form III was reported in 2015 by compressing form I above 2 GPa, but it reverts back to Form I when pressure is removed.[35] Form IV was reported in 2017. It is stable at ambient conditions.[36]
Mechanism of action
[edit]Discovery of the mechanism
[edit]In 1971, British pharmacologist John Robert Vane, then employed by the Royal College of Surgeons in London, showed aspirin suppressed the production of prostaglandins and thromboxanes.[37][38] For this discovery he was awarded the 1982 Nobel Prize in Physiology or Medicine, jointly with Sune Bergström and Bengt Ingemar Samuelsson.[39]
Prostaglandins and thromboxanes
[edit]Aspirin's ability to suppress the production of prostaglandins and thromboxanes is due to its irreversible inactivation of the cyclooxygenase (COX; officially known as prostaglandin-endoperoxide synthase, PTGS) enzyme required for prostaglandin and thromboxane synthesis. Aspirin acts as an acetylating agent where an acetyl group is covalently attached to a serine residue in the active site of the COX enzyme (Suicide inhibition). This makes aspirin different from other NSAIDs (such as diclofenac and ibuprofen), which are reversible inhibitors.
Low-dose aspirin use irreversibly blocks the formation of thromboxane A2 in platelets, producing an inhibitory effect on platelet aggregation during the lifetime of the affected platelet (8–9 days). This antithrombotic property makes aspirin useful for reducing the incidence of heart attacks in people who have had a heart attack, unstable angina, ischemic stroke or transient ischemic attack.[40] 40 mg of aspirin a day is able to inhibit a large proportion of maximum thromboxane A2 release provoked acutely, with the prostaglandin I2 synthesis being little affected; however, higher doses of aspirin are required to attain further inhibition.[41]
Prostaglandins, local hormones produced in the body, have diverse effects, including the transmission of pain information to the brain, modulation of the hypothalamic thermostat, and inflammation. Thromboxanes are responsible for the aggregation of platelets that form blood clots. Heart attacks are caused primarily by blood clots, and low doses of aspirin are seen as an effective medical intervention to prevent a second acute myocardial infarction.[42]
COX-1 and COX-2 inhibition
[edit]At least two different types of cyclooxygenases, COX-1 and COX-2, are acted on by aspirin. Aspirin irreversibly inhibits COX-1 and modifies the enzymatic activity of COX-2. COX-2 normally produces prostanoids, most of which are proinflammatory. Aspirin-modified COX-2 (aka prostaglandin-endoperoxide synthase 2 or PTGS2) produces epi-lipoxins, most of which are anti-inflammatory.[43][verification needed][44] Newer NSAID drugs, COX-2 inhibitors (coxibs), have been developed to inhibit only COX-2, with the intent to reduce the incidence of gastrointestinal side effects.[16]
Several COX-2 inhibitors, such as rofecoxib (Vioxx), have been withdrawn from the market, after evidence emerged that COX-2 inhibitors increase the risk of heart attack and stroke.[45][46] Endothelial cells lining the microvasculature in the body are proposed to express COX-2, and, by selectively inhibiting COX-2, prostaglandin production (specifically, PGI2; prostacyclin) is downregulated with respect to thromboxane levels, as COX-1 in platelets is unaffected. Thus, the protective anticoagulative effect of PGI2 is removed, increasing the risk of thrombus and associated heart attacks and other circulatory problems. Since platelets have no DNA, they are unable to synthesize new COX-1 once aspirin has irreversibly inhibited the enzyme, an important difference as compared with reversible inhibitors.
Furthermore, aspirin, while inhibiting the ability of COX-2 to form pro-inflammatory products such as the prostaglandins, converts this enzyme's activity from a prostaglandin-forming cyclooxygenase to a lipoxygenase-like enzyme: aspirin-treated COX-2 metabolizes a variety of polyunsaturated fatty acids to hydroperoxy products which are then further metabolized to specialized proresolving mediators such as the aspirin-triggered lipoxins(15-epilipoxin-A4/B4), aspirin-triggered resolvins, and aspirin-triggered maresins. These mediators possess potent anti-inflammatory activity. It is proposed that this aspirin-triggered transition of COX-2 from cyclooxygenase to lipoxygenase activity and the consequential formation of specialized proresolving mediators contributes to the anti-inflammatory effects of aspirin.[47][48][49]
Additional mechanisms
[edit]Aspirin has been shown to have at least three additional modes of action. It uncouples oxidative phosphorylation in cartilaginous (and hepatic) mitochondria, by diffusing from the inner membrane space as a proton carrier back into the mitochondrial matrix, where it ionizes once again to release protons.[50] Aspirin buffers and transports the protons. When high doses are given, it may actually cause fever, owing to the heat released from the electron transport chain, as opposed to the antipyretic action of aspirin seen with lower doses. In addition, aspirin induces the formation of NO-radicals in the body, which have been shown in mice to have an independent mechanism of reducing inflammation. This reduced leukocyte adhesion is an important step in the immune response to infection; however, evidence is insufficient to show aspirin helps to fight infection.[51] More recent data also suggest salicylic acid and its derivatives modulate signalling through NF-κB.[52] NF-κB, a transcription factor complex, plays a central role in many biological processes, including inflammation.[53][54][55]
Aspirin is readily broken down in the body to salicylic acid, which itself has anti-inflammatory, antipyretic, and analgesic effects. In 2012, salicylic acid was found to activate AMP-activated protein kinase, which has been suggested as a possible explanation for some of the effects of both salicylic acid and aspirin.[56][57] The acetyl portion of the aspirin molecule has its own targets. Acetylation of cellular proteins is a well-established phenomenon in the regulation of protein function at the post-translational level. Aspirin is able to acetylate several other targets in addition to COX isoenzymes.[58][59] These acetylation reactions may explain many hitherto unexplained effects of aspirin.[60]
Formulations
[edit]This section needs expansion. You can help by adding to it. (January 2023) |
Aspirin is produced in many formulations, with some differences in effect. In particular, aspirin can cause gastrointestinal bleeding, and formulations are sought which deliver the benefits of aspirin while mitigating harmful bleeding. Formulations may be combined (e.g., buffered + vitamin C).
- Tablets, typically of about 75–100 mg and 300–320 mg of immediate-release aspirin (IR-ASA).
- Dispersible tablets.
- Enteric-coated tablets.
- Buffered formulations containing aspirin with one of many buffering agents.
- Formulations of aspirin with vitamin C (ASA-VitC)
- A phospholipid-aspirin complex liquid formulation, PL-ASA. As of 2023[update] the phospholipid coating was being trialled to determine if it caused less gastrointestinal damage.[61]
Pharmacokinetics
[edit]Acetylsalicylic acid is a weak acid, and very little of it is ionized in the stomach after oral administration. Acetylsalicylic acid is quickly absorbed through the cell membrane in the acidic conditions of the stomach. The increased pH and larger surface area of the small intestine causes aspirin to be absorbed more slowly there, as more of it is ionized. Owing to the formation of concretions, aspirin is absorbed much more slowly during overdose, and plasma concentrations can continue to rise for up to 24 hours after ingestion.[62][63][64]
About 50–80% of salicylate in the blood is bound to human serum albumin, while the rest remains in the active, ionized state; protein binding is concentration-dependent. Saturation of binding sites leads to more free salicylate and increased toxicity. The volume of distribution is 0.1–0.2 L/kg. Acidosis increases the volume of distribution because of enhancement of tissue penetration of salicylates.[64]
As much as 80% of therapeutic doses of salicylic acid is metabolized in the liver. Conjugation with glycine forms salicyluric acid, and with glucuronic acid to form two different glucuronide esters. The conjugate with the acetyl group intact is referred to as the acyl glucuronide; the deacetylated conjugate is the phenolic glucuronide. These metabolic pathways have only a limited capacity. Small amounts of salicylic acid are also hydroxylated to gentisic acid. With large salicylate doses, the kinetics switch from first-order to zero-order, as metabolic pathways become saturated and renal excretion becomes increasingly important.[64]
Salicylates are excreted mainly by the kidneys as salicyluric acid (75%), free salicylic acid (10%), salicylic phenol (10%), and acyl glucuronides (5%), gentisic acid (< 1%), and 2,3-dihydroxybenzoic acid.[65] When small doses (less than 250 mg in an adult) are ingested, all pathways proceed by first-order kinetics, with an elimination half-life of about 2.0 h to 4.5 h.[66][67] When higher doses of salicylate are ingested (more than 4 g), the half-life becomes much longer (15 h to 30 h),[68] because the biotransformation pathways concerned with the formation of salicyluric acid and salicyl phenolic glucuronide become saturated.[69] Renal excretion of salicylic acid becomes increasingly important as the metabolic pathways become saturated, because it is extremely sensitive to changes in urinary pH. A 10- to 20-fold increase in renal clearance occurs when urine pH is increased from 5 to 8. The use of urinary alkalinization exploits this particular aspect of salicylate elimination.[70] It was found that short-term aspirin use in therapeutic doses might precipitate reversible acute kidney injury when the patient was ill with glomerulonephritis or cirrhosis.[71] Aspirin for some patients with chronic kidney disease and some children with congestive heart failure was contraindicated.[71]
History
[edit]
Medicines made from willow and other salicylate-rich plants appear in clay tablets from ancient Sumer as well as the Ebers Papyrus from ancient Egypt.[13]: 8–13 [21] Hippocrates referred to the use of salicylic tea to reduce fevers around 400 BC, and willow bark preparations were part of the pharmacopoeia of Western medicine in classical antiquity and the Middle Ages.[21] Willow bark extract became recognized for its specific effects on fever, pain, and inflammation in the mid-eighteenth century[72] after the Rev Edward Stone of Chipping Norton, Oxfordshire, noticed that the bitter taste of willow bark resembled the taste of the bark of the cinchona tree, known as "Peruvian bark", which was used successfully in Peru to treat a variety of ailments. Stone experimented with preparations of powdered willow bark on people in Chipping Norton for five years and found it to be as effective as Peruvian bark and a cheaper domestic version. In 1763 he sent a report of his findings to the Royal Society in London.[73] By the nineteenth century, pharmacists were experimenting with and prescribing a variety of chemicals related to salicylic acid, the active component of willow extract.[13]: 46–55

In 1853, chemist Charles Frédéric Gerhardt treated sodium salicylate with acetyl chloride to produce acetylsalicylic acid for the first time;[13]: 46–48 in the second half of the 19th century, other academic chemists established the compound's chemical structure and devised more efficient methods of synthesis. In 1897, scientists at the drug and dye firm Bayer began investigating acetylsalicylic acid as a less-irritating replacement for standard common salicylate medicines, and identified a new way to synthesize it.[13]: 69–75 That year, Felix Hoffmann (or Arthur Eichengrün) of Bayer was the first to produce acetylsalicylic acid in a pure, stable form.[14] By 1899, Bayer had dubbed this drug Aspirin and was selling it globally.[15]: 27 The word Aspirin was Bayer's brand name, rather than the generic name of the drug; however, Bayer's rights to the trademark were lost or sold in many countries. Aspirin's popularity grew over the first half of the 20th century leading to fierce competition with the proliferation of aspirin brands and products.[21]
Aspirin's popularity declined after the development of acetaminophen/paracetamol in 1956 and ibuprofen in 1962. In the 1960s and 1970s, John Vane and others discovered the basic mechanism of aspirin's effects,[13]: 226–231 while clinical trials and other studies from the 1960s to the 1980s established aspirin's efficacy as an anti-clotting agent that reduces the risk of clotting diseases.[13]: 247–257 The initial large studies on the use of low-dose aspirin to prevent heart attacks that were published in the 1970s and 1980s helped spur reform in clinical research ethics and guidelines for human subject research and US federal law, and are often cited as examples of clinical trials that included only men, but from which people drew general conclusions that did not hold true for women.[74][75][76]
Aspirin sales revived considerably in the last decades of the 20th century, and remain strong in the 21st century with widespread use as a preventive treatment for heart attacks and strokes.[13]: 267–269
Trademark
[edit]Bayer lost its trademark for Aspirin in the United States and some other countries in actions taken between 1918 and 1921 because it had failed to use the name for its own product correctly and had for years allowed the use of "Aspirin" by other manufacturers without defending the intellectual property rights.[77] Today, aspirin is a generic trademark in many countries.[78][79] Aspirin, with a capital "A", remains a registered trademark of Bayer in Germany, Canada, Mexico, and in over 80 other countries, for acetylsalicylic acid in all markets, but using different packaging and physical aspects for each.[80][81]
Compendial status
[edit]Medical use
[edit]Aspirin is used in the treatment of a number of conditions, including fever, pain, rheumatic fever, and inflammatory conditions, such as rheumatoid arthritis, pericarditis, and Kawasaki disease.[10] Lower doses of aspirin have also been shown to reduce the risk of death from a heart attack, or the risk of stroke in people who are at high risk or who have cardiovascular disease, but not in elderly people who are otherwise healthy.[84][85][86][87][88] There is evidence that aspirin is effective at preventing colorectal cancer, though the mechanisms of this effect are unclear.[89]
Pain
[edit]Aspirin is an effective analgesic for acute pain, although it is generally considered inferior to ibuprofen because aspirin is more likely to cause gastrointestinal bleeding.[90] Aspirin is generally ineffective for those pains caused by muscle cramps, bloating, gastric distension, or acute skin irritation.[91] As with other NSAIDs, combinations of aspirin and caffeine provide slightly greater pain relief than aspirin alone.[92] Effervescent formulations of aspirin relieve pain faster than aspirin in tablets,[93] which makes them useful for the treatment of migraines.[94] Topical aspirin may be effective for treating some types of neuropathic pain.[95]
Aspirin, either by itself or in a combined formulation, effectively treats certain types of a headache, but its efficacy may be questionable for others. Secondary headaches, meaning those caused by another disorder or trauma, should be promptly treated by a medical provider. Among primary headaches, the International Classification of Headache Disorders distinguishes between tension headache (the most common), migraine, and cluster headache. Aspirin or other over-the-counter analgesics are widely recognized as effective for the treatment of tension headaches.[96] Aspirin, especially as a component of an aspirin/paracetamol/caffeine combination, is considered a first-line therapy in the treatment of migraine, and comparable to lower doses of sumatriptan. It is most effective at stopping migraines when they are first beginning.[97]
Fever
[edit]Like its ability to control pain, aspirin's ability to control fever is due to its action on the prostaglandin system through its irreversible inhibition of COX.[98] Although aspirin's use as an antipyretic in adults is well established, many medical societies and regulatory agencies, including the American Academy of Family Physicians, the American Academy of Pediatrics, and the Food and Drug Administration, strongly advise against using aspirin for the treatment of fever in children because of the risk of Reye's syndrome, a rare but often fatal illness associated with the use of aspirin or other salicylates in children during episodes of viral or bacterial infection.[99][100][101] Because of the risk of Reye's syndrome in children, in 1986, the US Food and Drug Administration (FDA) required labeling on all aspirin-containing medications advising against its use in children and teenagers.[102]
Inflammation
[edit]Aspirin is used as an anti-inflammatory agent for both acute and long-term inflammation,[103] as well as for the treatment of inflammatory diseases, such as rheumatoid arthritis.[10]
Heart attacks and strokes
[edit]Aspirin is an important part of the treatment of those who have had a heart attack.[104] It is generally not recommended for routine use by people with no other health problems, including those over the age of 70.[105]
The 2009 Antithrombotic Trialists' Collaboration published in Lancet evaluated the efficacy and safety of low dose aspirin in secondary prevention. In those with prior ischaemic stroke or acute myocardial infarction, daily low dose aspirin was associated with a 19% relative risk reduction of serious cardiovascular events (non-fatal myocardial infarction, non-fatal stroke, or vascular death). This did come at the expense of a 0.19% absolute risk increase in gastrointestinal bleeding; however, the benefits outweigh the hazard risk in this case.[citation needed] Data from previous trials have suggested that weight-based dosing of aspirin has greater benefits in primary prevention of cardiovascular outcomes.[106] However, more recent trials were not able to replicate similar outcomes using low dose aspirin in low body weight (<70 kg) in specific subset of population studied i.e. elderly and diabetic population, and more evidence is required to study the effect of high dose aspirin in high body weight (≥70 kg).[107][108][109]
After percutaneous coronary interventions (PCIs), such as the placement of a coronary artery stent, a U.S. Agency for Healthcare Research and Quality guideline recommends that aspirin be taken indefinitely.[110] Frequently, aspirin is combined with an ADP receptor inhibitor, such as clopidogrel, prasugrel, or ticagrelor to prevent blood clots. This is called dual antiplatelet therapy (DAPT). Duration of DAPT was advised in the United States and European Union guidelines after the CURE[111] and PRODIGY[112] studies. In 2020, the systematic review and network meta-analysis from Khan et al.[113] showed promising benefits of short-term (< 6 months) DAPT followed by P2Y12 inhibitors in selected patients, as well as the benefits of extended-term (> 12 months) DAPT in high risk patients. In conclusion, the optimal duration of DAPT after PCIs should be personalized after outweighing each patient's risks of ischemic events and risks of bleeding events with consideration of multiple patient-related and procedure-related factors. Moreover, aspirin should be continued indefinitely after DAPT is complete.[114][115][116]
The status of the use of aspirin for the primary prevention in cardiovascular disease is conflicting and inconsistent, with recent changes from previously recommending it widely decades ago, and that some referenced newer trials in clinical guidelines show less of benefit of adding aspirin alongside other anti-hypertensive and cholesterol lowering therapies.[105][117] The ASCEND study demonstrated that in high-bleeding risk diabetics with no prior cardiovascular disease, there is no overall clinical benefit (12% decrease in risk of ischaemic events v/s 29% increase in GI bleeding) of low dose aspirin in preventing the serious vascular events over a period of 7.4 years. Similarly, the results of the ARRIVE study also showed no benefit of same dose of aspirin in reducing the time to first cardiovascular outcome in patients with moderate risk of cardiovascular disease over a period of five years. Aspirin has also been suggested as a component of a polypill for prevention of cardiovascular disease.[118][119] Complicating the use of aspirin for prevention is the phenomenon of aspirin resistance.[120][121] For people who are resistant, aspirin's efficacy is reduced.[122] Some authors have suggested testing regimens to identify people who are resistant to aspirin.[123]
As of April 2022[update], the United States Preventive Services Task Force (USPSTF) determined that there was a "small net benefit" for patients aged 40–59 with a 10% or greater 10-year cardiovascular disease (CVD) risk, and "no net benefit" for patients aged over 60.[124][125][126] Determining the net benefit was based on balancing the risk reduction of taking aspirin for heart attacks and ischaemic strokes, with the increased risk of gastrointestinal bleeding, intracranial bleeding, and hemorrhagic strokes. Their recommendations state that age changes the risk of the medicine, with the magnitude of the benefit of aspirin coming from starting at a younger age, while the risk of bleeding, while small, increases with age, particular for adults over 60, and can be compounded by other risk factors such as diabetes and a history of gastrointestinal bleeding. As a result, the USPSTF suggests that "people ages 40 to 59 who are at higher risk for CVD should decide with their clinician whether to start taking aspirin; people 60 or older should not start taking aspirin to prevent a first heart attack or stroke." Primary prevention guidelines from September 2019[update] made by the American College of Cardiology and the American Heart Association state they might consider aspirin for patients aged 40–69 with a higher risk of atherosclerotic CVD, without an increased bleeding risk, while stating they would not recommend aspirin for patients aged over 70 or adults of any age with an increased bleeding risk.[105] They state a CVD risk estimation and a risk discussion should be done before starting on aspirin, while stating aspirin should be used "infrequently in the routine primary prevention of (atherosclerotic CVD) because of lack of net benefit". As of August 2021[update], the European Society of Cardiology made similar recommendations; considering aspirin specifically to patients aged less than 70 at high or very high CVD risk, without any clear contraindications, on a case-by-case basis considering both ischemic risk and bleeding risk.[117]
Cancer prevention
[edit]Aspirin may reduce the overall risk of both getting cancer and dying from cancer.[127] There is substantial evidence for lowering the risk of colorectal cancer (CRC),[89][128][129][130] but aspirin must be taken for at least 10–20 years to see this benefit.[131] It may also slightly reduce the risk of endometrial cancer[132] and prostate cancer.[133]
Some conclude the benefits are greater than the risks due to bleeding in those at average risk.[127] Others are unclear if the benefits are greater than the risk.[134][135] Given this uncertainty, the 2007 United States Preventive Services Task Force (USPSTF) guidelines on this topic recommended against the use of aspirin for prevention of CRC in people with average risk.[136] Nine years later however, the USPSTF issued a grade B recommendation for the use of low-dose aspirin (75 to 100 mg/day) "for the primary prevention of CVD [cardiovascular disease] and CRC in adults 50 to 59 years of age who have a 10% or greater 10-year CVD risk, are not at increased risk for bleeding, have a life expectancy of at least 10 years, and are willing to take low-dose aspirin daily for at least 10 years".[137]
A meta-analysis through 2019 said that there was an association between taking aspirin and lower risk of cancer of the colorectum, esophagus, and stomach.[138]
In 2021, the U.S. Preventive services Task Force raised questions about the use of aspirin in cancer prevention. It notes the results of the 2018 ASPREE (Aspirin in Reducing Events in the Elderly) Trial, in which the risk of cancer-related death was higher in the aspirin-treated group than in the placebo group.[139]
Psychiatry
[edit]Bipolar disorder
[edit]Aspirin, along with several other agents with anti-inflammatory properties, has been repurposed as an add-on treatment for depressive episodes in subjects with bipolar disorder in light of the possible role of inflammation in the pathogenesis of severe mental disorders.[140] A 2022 systematic review concluded that aspirin exposure reduced the risk of depression in a pooled cohort of three studies (HR 0.624, 95% CI: 0.0503, 1.198, P=0.033). However, further high-quality, longer-duration, double-blind randomized controlled trials (RCTs) are needed to determine whether aspirin is an effective add-on treatment for bipolar depression.[141][142][143] Thus, notwithstanding the biological rationale, the clinical perspectives of aspirin and anti-inflammatory agents in the treatment of bipolar depression remain uncertain.[140]
Dementia
[edit]Although cohort and longitudinal studies have shown low-dose aspirin has a greater likelihood of reducing the incidence of dementia, numerous randomized controlled trials have not validated this.[144][145]
Schizophrenia
[edit]Some researchers have speculated the anti-inflammatory effects of aspirin may be beneficial for schizophrenia. Small trials have been conducted but evidence remains lacking.[146][147]
Other uses
[edit]Aspirin is a first-line treatment for the fever and joint-pain symptoms of acute rheumatic fever. The therapy often lasts for one to two weeks, and is rarely indicated for longer periods. After fever and pain have subsided, the aspirin is no longer necessary, since it does not decrease the incidence of heart complications and residual rheumatic heart disease.[148][149] Naproxen has been shown to be as effective as aspirin and less toxic, but due to the limited clinical experience, naproxen is recommended only as a second-line treatment.[148][150]
Along with rheumatic fever, Kawasaki disease remains one of the few indications for aspirin use in children[151] in spite of a lack of high quality evidence for its effectiveness.[152]
Low-dose aspirin supplementation has moderate benefits when used for prevention of pre-eclampsia.[153][154] This benefit is greater when started in early pregnancy.[155]
Aspirin has also demonstrated anti-tumoral effects, via inhibition of the PTTG1 gene, which is often overexpressed in tumors.[156]
Resistance
[edit]For some people, aspirin does not have as strong an effect on platelets as for others, an effect known as aspirin-resistance or insensitivity. One study has suggested women are more likely to be resistant than men,[157] and a different, aggregate study of 2,930 people found 28% were resistant.[158] A study in 100 Italian people found, of the apparent 31% aspirin-resistant subjects, only 5% were truly resistant, and the others were noncompliant.[159] Another study of 400 healthy volunteers found no subjects who were truly resistant, but some had "pseudoresistance, reflecting delayed and reduced drug absorption". [160]
Meta-analysis and systematic reviews have concluded that laboratory confirmed aspirin resistance confers increased rates of poorer outcomes in cardiovascular and neurovascular diseases.[161][158][162][163][164][165] Although the majority of research conducted has surrounded cardiovascular and neurovascular, there is emerging research into the risk of aspirin resistance after orthopaedic surgery where aspirin is used for venous thromboembolism prophylaxis.[166] Aspirin resistance in orthopaedic surgery, specifically after total hip and knee arthroplasties, is of interest as risk factors for aspirin resistance are also risk factors for venous thromboembolisms and osteoarthritis; the sequelae of requiring a total hip or knee arthroplasty. Some of these risk factors include obesity, advancing age, diabetes mellitus, dyslipidemia and inflammatory diseases.[166]
Dosages
[edit]Adult aspirin tablets are produced in standardised sizes, which vary slightly from country to country, for example 300 mg in Britain and 325 mg in the United States. Smaller doses are based on these standards, e.g., 75 mg and 81 mg tablets. The 81 mg tablets are commonly called "baby aspirin" or "baby-strength", because they were originally – but no longer – intended to be administered to infants and children.[167] No medical significance occurs due to the slight difference in dosage between the 75 mg and the 81 mg tablets. The dose required for benefit appears to depend on a person's weight.[106] For those weighing less than 70 kilograms (154 lb), low dose is effective for preventing cardiovascular disease; for patients above this weight, higher doses are required.[106]
In general, for adults, doses are taken four times a day for fever or arthritis,[168] with doses near the maximal daily dose used historically for the treatment of rheumatic fever.[169] For the prevention of myocardial infarction (MI) in someone with documented or suspected coronary artery disease, much lower doses are taken once daily.[168]
March 2009 recommendations from the USPSTF on the use of aspirin for the primary prevention of coronary heart disease encourage men aged 45–79 and women aged 55–79 to use aspirin when the potential benefit of a reduction in MI for men or stroke for women outweighs the potential harm of an increase in gastrointestinal hemorrhage.[170][171][needs update] The WHI study of postmenopausal women found that aspirin resulted in a 25% lower risk of death from cardiovascular disease and a 14% lower risk of death from any cause, though there was no significant difference between 81 mg and 325 mg aspirin doses.[172] The 2021 ADAPTABLE study also showed no significant difference in cardiovascular events or major bleeding between 81 mg and 325 mg doses of aspirin in patients (both men and women) with established cardiovascular disease.[173]
Low-dose aspirin use was also associated with a trend toward lower risk of cardiovascular events, and lower aspirin doses (75 or 81 mg/day) may optimize efficacy and safety for people requiring aspirin for long-term prevention.[171]
In children with Kawasaki disease, aspirin is taken at dosages based on body weight, initially four times a day for up to two weeks and then at a lower dose once daily for a further six to eight weeks.[174]
Adverse effects
[edit]In October 2020, the US Food and Drug Administration (FDA) required the drug label to be updated for all nonsteroidal anti-inflammatory medications to describe the risk of kidney problems in unborn babies that result in low amniotic fluid.[175][176] They recommend avoiding NSAIDs in pregnant women at 20 weeks or later in pregnancy.[175][176] One exception to the recommendation is the use of low-dose 81 mg aspirin at any point in pregnancy under the direction of a health care professional.[176]
Contraindications
[edit]Aspirin should not be taken by people who are allergic to ibuprofen or naproxen,[177][178] or who have salicylate intolerance[179][180] or a more generalized drug intolerance to NSAIDs, and caution should be exercised in those with asthma or NSAID-precipitated bronchospasm. Owing to its effect on the stomach lining, manufacturers recommend people with peptic ulcers, mild diabetes, or gastritis seek medical advice before using aspirin.[177][181] Even if none of these conditions is present, the risk of stomach bleeding is still increased when aspirin is taken with alcohol or warfarin.[177][178] People with hemophilia or other bleeding tendencies should not take aspirin or other salicylates.[177][181] Aspirin is known to cause hemolytic anemia in people who have the genetic disease glucose-6-phosphate dehydrogenase deficiency, particularly in large doses and depending on the severity of the disease.[182] Use of aspirin during dengue fever is not recommended owing to increased bleeding tendency.[183] Aspirin taken at doses of ≤325 mg and ≤100 mg per day for ≥2 days can increase the odds of suffering a gout attack by 81% and 91% respectively. This effect may potentially be worsened by high purine diets, diuretics, and kidney disease, but is eliminated by the urate lowering drug allopurinol.[184] Daily low dose aspirin does not appear to worsen kidney function.[185] Aspirin may reduce cardiovascular risk in those without established cardiovascular disease in people with moderate CKD, without significantly increasing the risk of bleeding.[186] Aspirin should not be given to children or adolescents under the age of 16 to control cold or influenza symptoms, as this has been linked with Reye's syndrome.[187]
Gastrointestinal
[edit]Aspirin increases the risk of upper gastrointestinal bleeding.[188] Enteric coating on aspirin may be used in manufacturing to prevent release of aspirin into the stomach to reduce gastric harm, but enteric coating does not reduce gastrointestinal bleeding risk.[188][189] Enteric-coated aspirin may not be as effective at reducing blood clot risk.[190][191] Combining aspirin with other NSAIDs has been shown to further increase the risk of gastrointestinal bleeding.[188] Using aspirin in combination with clopidogrel or warfarin also increases the risk of upper gastrointestinal bleeding.[192]
Blockade of COX-1 by aspirin apparently results in the upregulation of COX-2 as part of a gastric defense.[193] There is no clear evidence that simultaneous use of a COX-2 inhibitor with aspirin may increase the risk of gastrointestinal injury.[194]
"Buffering" is an additional method used with the intent to mitigate gastrointestinal bleeding, such as by preventing aspirin from concentrating in the walls of the stomach, although the benefits of buffered aspirin are disputed.[195] Almost any buffering agent used in antacids can be used; Bufferin, for example, uses magnesium oxide. Other preparations use calcium carbonate.[196] Gas-forming agents in effervescent tablet and powder formulations can also double as a buffering agent, one example being sodium bicarbonate, used in Alka-Seltzer.[197]
Taking vitamin C with aspirin has been investigated as a method of protecting the stomach lining. In trials vitamin C-releasing aspirin (ASA-VitC) or a buffered aspirin formulation containing vitamin C was found to cause less stomach damage than aspirin alone.[198][199]
Retinal vein occlusion
[edit]It is a widespread habit among eye specialists (ophthalmologists) to prescribe aspirin as an add-on medication for patients with retinal vein occlusion (RVO), such as central retinal vein occlusion (CRVO) and branch retinal vein occlusion (BRVO). The reason of this widespread use is the evidence of its proven effectiveness in major systemic venous thrombotic disorders, and it has been assumed that may be similarly beneficial in various types of retinal vein occlusion.
However, a large-scale investigation based on data of nearly 700 patients showed "that aspirin or other antiplatelet aggregating agents or anticoagulants adversely influence the visual outcome in patients with CRVO and hemi-CRVO, without any evidence of protective or beneficial effect".[200] Several expert groups, including the Royal College of Ophthalmologists, recommended against the use of antithrombotic drugs (incl. aspirin) for patients with RVO.[201]
Central effects
[edit]Large doses of salicylate, a metabolite of aspirin, cause temporary tinnitus (ringing in the ears) based on experiments in rats, via the action on arachidonic acid and NMDA receptors cascade.[202]
Reye's syndrome
[edit]Reye's syndrome, a rare but severe illness characterized by acute encephalopathy and fatty liver, can occur when children or adolescents are given aspirin for a fever or other illness or infection. From 1981 to 1997, 1207 cases of Reye's syndrome in people younger than 18 were reported to the US Centers for Disease Control and Prevention (CDC). Of these, 93% reported being ill in the three weeks preceding the onset of Reye's syndrome, most commonly with a respiratory infection, chickenpox, or diarrhea. Salicylates were detectable in 81.9% of children for whom test results were reported.[203] After the association between Reye's syndrome and aspirin was reported, and safety measures to prevent it (including a Surgeon General's warning, and changes to the labeling of aspirin-containing drugs) were implemented, aspirin taken by children declined considerably in the United States, as did the number of reported cases of Reye's syndrome; a similar decline was found in the United Kingdom after warnings against pediatric aspirin use were issued.[203] The US Food and Drug Administration recommends aspirin (or aspirin-containing products) should not be given to anyone under the age of 12 who has a fever,[187] and the UK National Health Service recommends children who are under 16 years of age should not take aspirin, unless it is on the advice of a doctor.[204]
Skin
[edit]For a small number of people, taking aspirin can result in symptoms including hives, swelling, and headache.[205] Aspirin can exacerbate symptoms among those with chronic hives, or create acute symptoms of hives.[206] These responses can be due to allergic reactions to aspirin, or more often due to its effect of inhibiting the COX-1 enzyme.[206][207] Skin reactions may also tie to systemic contraindications, seen with NSAID-precipitated bronchospasm,[206][207] or those with atopy.[208]
Aspirin and other NSAIDs, such as ibuprofen, may delay the healing of skin wounds.[209] Earlier findings from two small, low-quality trials suggested a benefit with aspirin (alongside compression therapy) on venous leg ulcer healing time and leg ulcer size,[210][211][212] however larger, more recent studies of higher quality have been unable to corroborate these outcomes.[213][214] As such, further research is required to clarify the role of aspirin in this context.
Other adverse effects
[edit]Aspirin can induce swelling of skin tissues in some people. In one study, angioedema appeared one to six hours after ingesting aspirin in some of the people. However, when the aspirin was taken alone, it did not cause angioedema in these people; the aspirin had been taken in combination with another NSAID-induced drug when angioedema appeared.[215]
Aspirin causes an increased risk of cerebral microbleeds, having the appearance on MRI scans of 5 to 10 mm or smaller, hypointense (dark holes) patches.[216][217]
A study of a group with a mean dosage of aspirin of 270 mg per day estimated an average absolute risk increase in intracerebral hemorrhage (ICH) of 12 events per 10,000 persons.[218] In comparison, the estimated absolute risk reduction in myocardial infarction was 137 events per 10,000 persons, and a reduction of 39 events per 10,000 persons in ischemic stroke.[218] In cases where ICH already has occurred, aspirin use results in higher mortality, with a dose of about 250 mg per day resulting in a relative risk of death within three months after the ICH around 2.5 (95% confidence interval 1.3 to 4.6).[219]
Aspirin and other NSAIDs can cause abnormally high blood levels of potassium by inducing a hyporeninemic hypoaldosteronism state via inhibition of prostaglandin synthesis; however, these agents do not typically cause hyperkalemia by themselves in the setting of normal renal function and euvolemic state.[220]
Use of low-dose aspirin before a surgical procedure has been associated with an increased risk of bleeding events in some patients, however, ceasing aspirin prior to surgery has also been associated with an increase in major adverse cardiac events. An analysis of multiple studies found a three-fold increase in adverse events such as myocardial infarction in patients who ceased aspirin prior to surgery. The analysis found that the risk is dependent on the type of surgery being performed and the patient indication for aspirin use.[221]
On 9 July 2015, the US Food and Drug Administration (FDA) toughened warnings of increased heart attack and stroke risk associated with nonsteroidal anti-inflammatory drugs (NSAID).[222] Aspirin is an NSAID but is not affected by the new warnings.[222]
Overdose
[edit]Aspirin overdose can be acute or chronic. In acute poisoning, a single large dose is taken; in chronic poisoning, higher than normal doses are taken over a period of time. Acute overdose has a mortality rate of 2%. Chronic overdose is more commonly lethal, with a mortality rate of 25%;[223] chronic overdose may be especially severe in children.[224] Toxicity is managed with a number of potential treatments, including activated charcoal, intravenous dextrose and normal saline, sodium bicarbonate, and dialysis.[225] The diagnosis of poisoning usually involves measurement of plasma salicylate, the active metabolite of aspirin, by automated spectrophotometric methods. Plasma salicylate levels in general range from 30 to 100 mg/L after usual therapeutic doses, 50–300 mg/L in people taking high doses and 700–1400 mg/L following acute overdose. Salicylate is also produced as a result of exposure to bismuth subsalicylate, methyl salicylate, and sodium salicylate.[226][227]
Interactions
[edit]Aspirin is known to interact with other drugs. For example, acetazolamide and ammonium chloride are known to enhance the intoxicating effect of salicylates, and alcohol also increases the gastrointestinal bleeding associated with these types of drugs.[177][178] Aspirin is known to displace a number of drugs from protein-binding sites in the blood, including the antidiabetic drugs tolbutamide and chlorpropamide, warfarin, methotrexate, phenytoin, probenecid, valproic acid (as well as interfering with beta oxidation, an important part of valproate metabolism), and other NSAIDs. Corticosteroids may also reduce the concentration of aspirin. Other NSAIDs, such as ibuprofen and naproxen, may reduce the antiplatelet effect of aspirin.[228][229] Although limited evidence suggests this may not result in a reduced cardioprotective effect of aspirin.[228] Analgesic doses of aspirin decrease sodium loss induced by spironolactone in the urine, however this does not reduce the antihypertensive effects of spironolactone.[230] Furthermore, antiplatelet doses of aspirin are deemed too small to produce an interaction with spironolactone.[231] Aspirin is known to compete with penicillin G for renal tubular secretion.[232] Aspirin may also inhibit the absorption of vitamin C.[233][234][unreliable medical source?][235]
Research
[edit]The ISIS-2 trial demonstrated that aspirin at doses of 160 mg daily for one month, decreased the mortality by 21% of participants with a suspected myocardial infarction in the first five weeks.[236] A single daily dose of 324 mg of aspirin for 12 weeks has a highly protective effect against acute myocardial infarction and death in men with unstable angina.[237]
Bipolar disorder
[edit]Aspirin has been repurposed as an add-on treatment for depressive episodes in subjects with bipolar disorder.[140] However, meta-analytic evidence is based on very few studies and does not suggest any efficacy of aspirin in the treatment of bipolar depression.[140] Thus, notwithstanding the biological rationale, the clinical perspectives of aspirin and anti-inflammatory agents in the treatment of bipolar depression remain uncertain.[140]
Infectious diseases
[edit]Several studies investigated the anti-infective properties of aspirin for bacterial, viral and parasitic infections. Aspirin was demonstrated to limit platelet activation induced by Staphylococcus aureus and Enterococcus faecalis and to reduce streptococcal adhesion to heart valves. In patients with tuberculous meningitis, the addition of aspirin reduced the risk of new cerebral infarction [RR = 0.52 (0.29-0.92)]. A role of aspirin on bacterial and fungal biofilm is also being supported by growing evidence.[238]
Cancer prevention
[edit]Evidence from observational studies was conflicting on the effect of aspirin in breast cancer prevention;[239] a randomized controlled trial showed that aspirin had no significant effect in reducing breast cancer,[240] thus further studies are needed to clarify the effect of aspirin in cancer prevention.
In gardening
[edit]There are many anecdotal reportings that aspirin can improve plant's growth and resistance[241][242] though most research involved salicylic acid instead of aspirin.[243]
Veterinary medicine
[edit]Aspirin is sometimes used in veterinary medicine as an anticoagulant or to relieve pain associated with musculoskeletal inflammation or osteoarthritis. Aspirin should be given to animals only under the direct supervision of a veterinarian, as adverse effects—including gastrointestinal issues—are common. An aspirin overdose in any species may result in salicylate poisoning, characterized by hemorrhaging, seizures, coma, and even death.[244]
Dogs are better able to tolerate aspirin than cats are.[245] Cats metabolize aspirin slowly because they lack the glucuronide conjugates that aid in the excretion of aspirin, making it potentially toxic if dosing is not spaced out properly.[244][246] No clinical signs of toxicosis occurred when cats were given 25 mg/kg of aspirin every 48 hours for 4 weeks,[245] but the recommended dose for relief of pain and fever and for treating blood clotting diseases in cats is 10 mg/kg every 48 hours to allow for metabolization.[244][247]
References
[edit]- ^ McTavish J (Fall 1987). "What's in a Name? Aspirin and the American Medical Association". Bulletin of the History of Medicine. 61 (3): 343–366. JSTOR 44442097. PMID 3311247.
- ^ "Aspirin Use During Pregnancy". Drugs.com. 2 April 2018. Retrieved 29 December 2019.
- ^ "OTC medicine monograph: Aspirin tablets for oral use". Therapeutic Goods Administration (TGA). 21 June 2022. Retrieved 4 April 2023.
- ^ "Poisons Standard October 2022". Australian Government Federal Register of Legislation. 26 September 2022. Retrieved 9 January 2023.
- ^ "Aspirin Product information". Health Canada. 22 October 2009. Retrieved 20 August 2023.
- ^ a b "Zorprin, Bayer Buffered Aspirin (aspirin) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Archived from the original on 7 April 2014. Retrieved 3 April 2014.
- ^ a b c Brayfield A, ed. (14 January 2014). "Aspirin". Martindale: The Complete Drug Reference. Pharmaceutical Press. Retrieved 3 April 2014.
- ^ CID 2244 from PubChem
- ^ a b Haynes WM, ed. (2011). CRC Handbook of Chemistry and Physics (92nd ed.). Boca Raton, Florida: CRC Press. p. 3.8. ISBN 1-4398-5511-0.
- ^ a b c d e f g h i j k l m n "Aspirin". American Society of Health-System Pharmacists. 29 November 2021. Archived from the original on 25 April 2017 – via Drugs.com.
- ^ a b Jones A (2015). Chemistry: An Introduction for Medical and Health Sciences. John Wiley & Sons. pp. 5–6. ISBN 978-0-470-09290-3.
- ^ Ravina E (2011). The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs. John Wiley & Sons. p. 24. ISBN 978-3-527-32669-3.
- ^ a b c d e f g h i j Jeffreys D (2008). Aspirin the remarkable story of a wonder drug. Bloomsbury Publishing USA. ISBN 978-1-59691-816-0. Archived from the original on 8 September 2017.: 46–48
- ^ a b "Felix Hoffmann". Science History Institute. Retrieved 3 October 2024.
- ^ a b c Mann CC, Plummer ML (1991). The aspirin wars: money, medicine, and 100 years of rampant competition (1st ed.). New York: Knopf. p. 27. ISBN 978-0-394-57894-1.
- ^ a b Warner TD, Mitchell JA (October 2002). "Cyclooxygenase-3 (COX-3): filling in the gaps toward a COX continuum?". Proceedings of the National Academy of Sciences of the United States of America. 99 (21): 13371–3. Bibcode:2002PNAS...9913371W. doi:10.1073/pnas.222543099. PMC 129677. PMID 12374850.
- ^ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ^ "The Top 300 of 2022". ClinCalc. Archived from the original on 30 August 2024. Retrieved 30 August 2024.
- ^ "Aspirin Drug Usage Statistics, United States, 2013 - 2022". ClinCalc. Retrieved 30 August 2024.
- ^ Dick B (2018). "Hard Work and Happenstance". Distillations. Vol. 4, no. 1. Science History Institute. pp. 44–45.
- ^ a b c d e "Aspirin". Chemical & Engineering News. Vol. 83, no. 25. 20 June 2005.
- ^ Reynolds EF, ed. (1982). "Aspirin and similar analgesic and anti-inflammatory agents". Martindale: the extra pharmacopoeia (28th ed.). Rittenhouse Book Distributors. pp. 234–82. ISBN 978-0-85369-160-0.
- ^ "Acetylsalicylic acid". NIOSH Pocket Guide to Chemical Hazards. U.S. National Institute for Occupational Safety and Health (NIOSH). 11 April 2016. Archived from the original on 11 May 2017.
- ^ "Appendix G: 1989 Air contaminants update project – Exposure limits NOT in effect". NIOSH pocket guide to chemical hazards. National Institute for Occupational Safety and Health. 13 February 2015. Archived from the original on 18 June 2017.
- ^ Palleros DR (2000). Experimental organic chemistry. New York: John Wiley & Sons. p. 494. ISBN 978-0-471-28250-1.
- ^ "Chemical of the Week -- Acetic Acid and Acetic Anhydride". www.eng.uwaterloo.ca. Archived from the original on 3 November 2022.
- ^ Barrans R (18 May 2008). "Aspirin aging". Newton BBS. Archived from the original on 18 May 2008.
- ^ Carstensen JT, Attarchi F (April 1988). "Decomposition of aspirin in the solid state in the presence of limited amounts of moisture III: Effect of temperature and a possible mechanism". Journal of Pharmaceutical Sciences. 77 (4): 318–21. doi:10.1002/jps.2600770407. PMID 3379589.
- ^ Myers RL (2007). The 100 most important chemical compounds: a reference guide. ABC-CLIO. p. 10. ISBN 978-0-313-33758-1. Archived from the original on 10 June 2013.
- ^ "Acetylsalicylic acid". Jinno Laboratory, School of Materials Science, Toyohashi University of Technology. 4 March 1996. Archived from the original on 20 January 2012. Retrieved 12 April 2014.
- ^ a b Bučar DK, Lancaster RW, Bernstein J (June 2015). "Disappearing polymorphs revisited". Angewandte Chemie. 54 (24): 6972–6993. doi:10.1002/anie.201410356. PMC 4479028. PMID 26031248.
- ^ Vishweshwar P, McMahon JA, Oliveira M, Peterson ML, Zaworotko MJ (December 2005). "The predictably elusive form II of aspirin". Journal of the American Chemical Society. 127 (48): 16802–16803. doi:10.1021/ja056455b. PMID 16316223.
- ^ Bond AD, Boese R, Desiraju GR (2007). "On the polymorphism of aspirin: crystalline aspirin as intergrowths of two "polymorphic" domains". Angewandte Chemie. 46 (4): 618–622. doi:10.1002/anie.200603373. PMID 17139692.
- ^ "Polytypism - Online Dictionary of Crystallography". reference.iucr.org.
- ^ Crowell EL, Dreger ZA, Gupta YM (15 February 2015). "High-pressure polymorphism of acetylsalicylic acid (aspirin): Raman spectroscopy". Journal of Molecular Structure. 1082: 29–37. Bibcode:2015JMoSt1082...29C. doi:10.1016/j.molstruc.2014.10.079. ISSN 0022-2860.
- ^ Shtukenberg AG, Hu CT, Zhu Q, Schmidt MU, Xu W, Tan M, et al. (7 June 2017). "The Third Ambient Aspirin Polymorph". Crystal Growth & Design. 17 (6): 3562–3566. doi:10.1021/acs.cgd.7b00673. ISSN 1528-7483. OSTI 1373897.
- ^ Vane JR (June 1971). "Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs". Nature. 231 (25): 232–5. doi:10.1038/newbio231232a0. PMID 5284360.
- ^ Vane JR, Botting RM (June 2003). "The mechanism of action of aspirin". Thrombosis Research. 110 (5–6): 255–8. doi:10.1016/s0049-3848(03)00379-7. PMID 14592543.
- ^ "The Nobel Prize in Physiology or Medicine 1982". Nobelprize.org. Archived from the original on 27 June 2017.
- ^ "Aspirin in heart attack and stroke prevention". American Heart Association. Archived from the original on 31 March 2008. Retrieved 8 May 2008.
- ^ Tohgi H, Konno S, Tamura K, Kimura B, Kawano K (October 1992). "Effects of low-to-high doses of aspirin on platelet aggregability and metabolites of thromboxane A2 and prostacyclin". Stroke. 23 (10): 1400–3. doi:10.1161/01.STR.23.10.1400. PMID 1412574.
- ^ Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, et al. (May 2009). "Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials". Lancet. 373 (9678): 1849–60. doi:10.1016/S0140-6736(09)60503-1. PMC 2715005. PMID 19482214.
- ^ Goel A, Aggarwal S, Partap S, Saurabh A, Choudhary (2012). "Pharmacokinetic solubility and dissolution profile of antiarrythmic drugs". Int J Pharma Prof Res. 3 (1): 592–601.
- ^ Clària J, Serhan CN (October 1995). "Aspirin triggers previously undescribed bioactive eicosanoids by human endothelial cell-leukocyte interactions". Proceedings of the National Academy of Sciences of the United States of America. 92 (21): 9475–9479. Bibcode:1995PNAS...92.9475C. doi:10.1073/pnas.92.21.9475. PMC 40824. PMID 7568157.
- ^ Martínez-González J, Badimon L (2007). "Mechanisms underlying the cardiovascular effects of COX-inhibition: benefits and risks". Current Pharmaceutical Design. 13 (22): 2215–27. doi:10.2174/138161207781368774. PMID 17691994.
- ^ Funk CD, FitzGerald GA (November 2007). "COX-2 inhibitors and cardiovascular risk". Journal of Cardiovascular Pharmacology. 50 (5): 470–9. doi:10.1097/FJC.0b013e318157f72d. PMID 18030055. S2CID 39103383.
- ^ Romano M, Cianci E, Simiele F, Recchiuti A (August 2015). "Lipoxins and aspirin-triggered lipoxins in resolution of inflammation". European Journal of Pharmacology. 760: 49–63. doi:10.1016/j.ejphar.2015.03.083. PMID 25895638.
- ^ Serhan CN, Chiang N (August 2013). "Resolution phase lipid mediators of inflammation: agonists of resolution". Current Opinion in Pharmacology. 13 (4): 632–40. doi:10.1016/j.coph.2013.05.012. PMC 3732499. PMID 23747022.
- ^ Weylandt KH (August 2016). "Docosapentaenoic acid derived metabolites and mediators - The new world of lipid mediator medicine in a nutshell". European Journal of Pharmacology. 785: 108–115. doi:10.1016/j.ejphar.2015.11.002. PMID 26546723.
- ^ Somasundaram S, Sigthorsson G, Simpson RJ, Watts J, Jacob M, Tavares IA, et al. (May 2000). "Uncoupling of intestinal mitochondrial oxidative phosphorylation and inhibition of cyclooxygenase are required for the development of NSAID-enteropathy in the rat". Alimentary Pharmacology & Therapeutics. 14 (5): 639–50. doi:10.1046/j.1365-2036.2000.00723.x. PMID 10792129. S2CID 44832283.
- ^ Paul-Clark MJ, Van Cao T, Moradi-Bidhendi N, Cooper D, Gilroy DW (July 2004). "15-epi-lipoxin A4-mediated induction of nitric oxide explains how aspirin inhibits acute inflammation". The Journal of Experimental Medicine. 200 (1): 69–78. doi:10.1084/jem.20040566. PMC 2213311. PMID 15238606.
- ^ McCarty MF, Block KI (September 2006). "Preadministration of high-dose salicylates, suppressors of NF-kappaB activation, may increase the chemosensitivity of many cancers: an example of proapoptotic signal modulation therapy". Integrative Cancer Therapies. 5 (3): 252–68. doi:10.1177/1534735406291499. PMID 16880431.
- ^ Silva Caldas AP, Chaves LO, Linhares Da Silva L, De Castro Morais D, Gonçalves Alfenas RD (29 December 2017). "Mechanisms involved in the cardioprotective effect of avocado consumption: A systematic review". International Journal of Food Properties. 20 (sup2): 1675–1685. doi:10.1080/10942912.2017.1352601. ISSN 1094-2912.
...there was postprandial reduction on the plasma concentration of IL-6 and IkBα preservation, followed by the lower activation of NFκB, considered the main transcription factor capable of inducing inflammatory response by stimulating the expression of proinflammatory cytokines, chemokines, and adhesion molecules.
- ^ Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, et al. (January 2018). "Inflammatory responses and inflammation-associated diseases in organs". Oncotarget. 9 (6): 7204–7218. doi:10.18632/oncotarget.23208. PMC 5805548. PMID 29467962.
- ^ Lawrence T (December 2009). "The nuclear factor NF-kappaB pathway in inflammation". Cold Spring Harbor Perspectives in Biology. 1 (6): a001651. doi:10.1101/cshperspect.a001651. PMC 2882124. PMID 20457564.
- ^ Hawley SA, Fullerton MD, Ross FA, Schertzer JD, Chevtzoff C, Walker KJ, et al. (May 2012). "The ancient drug salicylate directly activates AMP-activated protein kinase". Science. 336 (6083): 918–22. Bibcode:2012Sci...336..918H. doi:10.1126/science.1215327. PMC 3399766. PMID 22517326.
- ^ "Clues to aspirin's anti-cancer effects revealed". New Scientist. 214 (2862): 16. 28 April 2012. doi:10.1016/S0262-4079(12)61073-2.
- ^ Alfonso LF, Srivenugopal KS, Arumugam TV, Abbruscato TJ, Weidanz JA, Bhat GJ (March 2009). "Aspirin inhibits camptothecin-induced p21CIP1 levels and potentiates apoptosis in human breast cancer cells". International Journal of Oncology. 34 (3): 597–608. doi:10.3892/ijo_00000185. PMID 19212664.
- ^ Alfonso LF, Srivenugopal KS, Bhat GJ (2009). "Does aspirin acetylate multiple cellular proteins? (Review)". Molecular Medicine Reports (review). 2 (4): 533–7. doi:10.3892/mmr_00000132. PMID 21475861.
- ^ Alfonso LF, Srivenugopal KS, Bhat GJ (4 June 2009). "Does aspirin acetylate multiple cellular proteins? (Review)". Molecular Medicine Reports. 2 (4): 533–537. doi:10.3892/mmr_00000132. PMID 21475861.
- ^ Franchi F, Schneider D, Prats J, Fan W, Rollini F, Been L, et al. (2021). "TCT-320 Pharmacokinetic and Pharmacodynamic Profile of PL-ASA, a Novel Phospholipid-Aspirin Complex Liquid Formulation, Compared to Enteric-Coated Aspirin at an 81-mg Dose – Results From a Prospective, Randomized, Crossover Study". Journal of the American College of Cardiology. 78 (19). Elsevier BV: B131. doi:10.1016/j.jacc.2021.09.1173. ISSN 0735-1097.
- ^ Ferguson RK, Boutros AR (August 1970). "Death following self-poisoning with aspirin". JAMA. 213 (7): 1186–8. doi:10.1001/jama.213.7.1186. PMID 5468267.
- ^ Kaufman FL, Dubansky AS (April 1972). "Darvon poisoning with delayed salicylism: a case report". Pediatrics. 49 (4): 610–1. doi:10.1542/peds.49.4.610. PMID 5013423. S2CID 29427204.
- ^ a b c Levy G, Tsuchiya T (August 1972). "Salicylate accumulation kinetics in man". The New England Journal of Medicine. 287 (9): 430–2. doi:10.1056/NEJM197208312870903. PMID 5044917.
- ^ Grootveld M, Halliwell B (January 1988). "2,3-Dihydroxybenzoic acid is a product of human aspirin metabolism". Biochemical Pharmacology. 37 (2): 271–80. doi:10.1016/0006-2952(88)90729-0. PMID 3342084.
- ^ Hartwig-Otto H (November 1983). "Pharmacokinetic considerations of common analgesics and antipyretics". The American Journal of Medicine. 75 (5A): 30–7. doi:10.1016/0002-9343(83)90230-9. PMID 6606362.
- ^ Done AK (November 1960). "Salicylate intoxication. Significance of measurements of salicylate in blood in cases of acute ingestion". Pediatrics. 26: 800–7. doi:10.1542/peds.26.5.800. PMID 13723722. S2CID 245036862.
- ^ Chyka PA, Erdman AR, Christianson G, Wax PM, Booze LL, Manoguerra AS, et al. (2007). "Salicylate poisoning: an evidence-based consensus guideline for out-of-hospital management". Clinical Toxicology. 45 (2): 95–131. doi:10.1080/15563650600907140. PMID 17364628.
- ^ Prescott LF, Balali-Mood M, Critchley JA, Johnstone AF, Proudfoot AT (November 1982). "Diuresis or urinary alkalinisation for salicylate poisoning?". British Medical Journal. 285 (6352): 1383–6. doi:10.1136/bmj.285.6352.1383. PMC 1500395. PMID 6291695.
- ^ Dargan PI, Wallace CI, Jones AL (May 2002). "An evidence based flowchart to guide the management of acute salicylate (aspirin) overdose". Emergency Medicine Journal. 19 (3): 206–9. doi:10.1136/emj.19.3.206. PMC 1725844. PMID 11971828.
- ^ a b D'Agati V (July 1996). "Does aspirin cause acute or chronic renal failure in experimental animals and in humans?". American Journal of Kidney Diseases. 28 (1 Suppl 1): S24-9. doi:10.1016/s0272-6386(96)90565-x. PMID 8669425.
- ^ Goldberg DR (Summer 2009). "Aspirin: Turn of the Century Miracle Drug". Chemical Heritage. Vol. 27, no. 2. pp. 26–30.
- ^ Diarmuid Jeffreys (2004). Aspirin: the Remarkable Story of a Wonder Drug. Bloomsbury. p. 18-34.
- ^ Schiebinger L (October 2003). "Women's health and clinical trials". The Journal of Clinical Investigation. 112 (7): 973–7. doi:10.1172/JCI19993. PMC 198535. PMID 14523031.
- ^ "Regular aspirin intake and acute myocardial infarction". British Medical Journal. 1 (5905): 440–3. March 1974. doi:10.1136/bmj.1.5905.440. PMC 1633212. PMID 4816857.
- ^ Elwood PC, Cochrane AL, Burr ML, Sweetnam PM, Williams G, Welsby E, et al. (March 1974). "A randomized controlled trial of acetyl salicylic acid in the secondary prevention of mortality from myocardial infarction". British Medical Journal. 1 (5905): 436–40. doi:10.1136/bmj.1.5905.436. PMC 1633246. PMID 4593555.
- ^ Bayer Co. v. United Drug Co., 272 F. 505, p.512 (S.D.N.Y 1921).
- ^ "Has aspirin become a generic trademark?". genericides.org. 25 March 2020. Archived from the original on 5 March 2021. Retrieved 17 February 2021.
- ^ Huth EJ, et al. (CBE Style Manual Committee) (1994). Scientific style and format: the CBE manual for authors, editors, and publishers. Cambridge University Press. p. 164. Bibcode:1994ssfc.book.....S. ISBN 978-0-521-47154-1. Archived from the original on 15 October 2015.
- ^ "Aspirin: the versatile drug". CBC News. 28 May 2009. Archived from the original on 6 November 2016.
- ^ Cheng TO (2007). "The history of aspirin". Texas Heart Institute Journal. 34 (3): 392–3. PMC 1995051. PMID 17948100.
- ^ "Aspirin". Sigma Aldrich. Retrieved 24 January 2022.
- ^ "Index BP 2009" (PDF). British Pharmacopoeia. Archived from the original (PDF) on 11 April 2009. Retrieved 13 July 2009.
- ^
 This article incorporates text from this source, which is in the public domain: "Aspirin for reducing your risk of heart attack and stroke: know the facts". U.S. Food and Drug Administration (FDA). Archived from the original on 14 August 2012. Retrieved 26 July 2012.
This article incorporates text from this source, which is in the public domain: "Aspirin for reducing your risk of heart attack and stroke: know the facts". U.S. Food and Drug Administration (FDA). Archived from the original on 14 August 2012. Retrieved 26 July 2012.
- ^
 This article incorporates text from this source, which is in the public domain: "Aspirin for the prevention of cardiovascular disease". U.S. Preventive Services Task Force. Archived from the original on 11 July 2012. Retrieved 26 July 2012.
This article incorporates text from this source, which is in the public domain: "Aspirin for the prevention of cardiovascular disease". U.S. Preventive Services Task Force. Archived from the original on 11 July 2012. Retrieved 26 July 2012.
- ^ Seshasai SR, Wijesuriya S, Sivakumaran R, Nethercott S, Erqou S, Sattar N, et al. (February 2012). "Effect of aspirin on vascular and nonvascular outcomes: meta-analysis of randomized controlled trials". Archives of Internal Medicine. 172 (3): 209–16. doi:10.1001/archinternmed.2011.628. hdl:10044/1/34287. PMID 22231610.
- ^ McNeil JJ, Woods RL, Nelson MR, Reid CM, Kirpach B, Wolfe R, et al. (October 2018). "Effect of Aspirin on Disability-free Survival in the Healthy Elderly". The New England Journal of Medicine. 379 (16): 1499–1508. doi:10.1056/NEJMoa1800722. hdl:1885/154654. PMC 6426126. PMID 30221596.
- ^ McNeil JJ, Wolfe R, Woods RL, Tonkin AM, Donnan GA, Nelson MR, et al. (October 2018). "Effect of Aspirin on Cardiovascular Events and Bleeding in the Healthy Elderly". The New England Journal of Medicine. 379 (16): 1509–1518. doi:10.1056/NEJMoa1805819. PMC 6289056. PMID 30221597.
- ^ a b Algra AM, Rothwell PM (May 2012). "Effects of regular aspirin on long-term cancer incidence and metastasis: a systematic comparison of evidence from observational studies versus randomised trials". The Lancet. Oncology. 13 (5): 518–27. doi:10.1016/S1470-2045(12)70112-2. PMID 22440112.
- ^ Sachs CJ (March 2005). "Oral analgesics for acute nonspecific pain". American Family Physician. 71 (5): 913–8. PMID 15768621.
- ^ Gaciong Z (June 2003). "The real dimension of analgesic activity of aspirin". Thrombosis Research. 110 (5–6): 361–4. doi:10.1016/j.thromres.2003.08.009. PMID 14592563.
- ^ Derry CJ, Derry S, Moore RA (December 2014). "Caffeine as an analgesic adjuvant for acute pain in adults". The Cochrane Database of Systematic Reviews. 2014 (12): CD009281. doi:10.1002/14651858.CD009281.pub3. PMC 6485702. PMID 25502052.
- ^ Hersh EV, Moore PA, Ross GL (May 2000). "Over-the-counter analgesics and antipyretics: a critical assessment". Clinical Therapeutics. 22 (5): 500–48. doi:10.1016/S0149-2918(00)80043-0. PMID 10868553.
- ^ Mett A, Tfelt-Hansen P (June 2008). "Acute migraine therapy: recent evidence from randomized comparative trials". Current Opinion in Neurology. 21 (3): 331–7. doi:10.1097/WCO.0b013e3282fee843. PMID 18451718. S2CID 44459366.
- ^ Kingery WS (November 1997). "A critical review of controlled clinical trials for peripheral neuropathic pain and complex regional pain syndromes". Pain. 73 (2): 123–139. doi:10.1016/S0304-3959(97)00049-3. PMID 9415498. S2CID 10418793.
- ^ Loder E, Rizzoli P (January 2008). "Tension-type headache". BMJ. 336 (7635): 88–92. doi:10.1136/bmj.39412.705868.AD. PMC 2190284. PMID 18187725.
- ^ Gilmore B, Michael M (February 2011). "Treatment of acute migraine headache". American Family Physician. 83 (3): 271–80. PMID 21302868.
- ^ Bartfai T, Conti B (March 2010). "Fever". TheScientificWorldJournal. 10: 490–503. doi:10.1100/tsw.2010.50. PMC 2850202. PMID 20305990.
- ^ Pugliese A, Beltramo T, Torre D (October 2008). "Reye's and Reye's-like syndromes". Cell Biochemistry and Function. 26 (7): 741–6. doi:10.1002/cbf.1465. PMID 18711704. S2CID 22361194.
- ^ Beutler AI, Chesnut GT, Mattingly JC, Jamieson B (December 2009). "FPIN's Clinical Inquiries. Aspirin use in children for fever or viral syndromes". American Family Physician. 80 (12): 1472. PMID 20000310.
- ^ "Medications Used to Treat Fever". American Academy of Pediatrics. 29 June 2012. Archived from the original on 18 February 2013. Retrieved 25 November 2012.
- ^ "51 FR 8180" (PDF). United States Federal Register. 51 (45). 7 March 1986. Archived from the original (PDF) on 19 August 2011.
- ^ Morris T, Stables M, Hobbs A, de Souza P, Colville-Nash P, Warner T, et al. (August 2009). "Effects of low-dose aspirin on acute inflammatory responses in humans". Journal of Immunology. 183 (3): 2089–96. doi:10.4049/jimmunol.0900477. PMID 19597002.
- ^ National Clinical Guideline Centre (UK) (July 2013). "Adjunctive pharmacotherapy and associated NICE guidance". Myocardial infarction with ST-segment elevation: the acute management of myocardial infarction with ST-segment elevation [Internet]. NICE Clinical Guidelines. Royal College of Physicians (UK). 17.2 Aspirin. PMID 25340241. Archived from the original on 31 December 2015.
- ^ a b c Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. (September 2019). "2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Journal of the American College of Cardiology. 74 (10): e177–e232. doi:10.1016/j.jacc.2019.03.010. PMC 7685565. PMID 30894318.
- ^ a b c Rothwell PM, Cook NR, Gaziano JM, Price JF, Belch JF, Roncaglioni MC, et al. (August 2018). "Effects of aspirin on risks of vascular events and cancer according to bodyweight and dose: analysis of individual patient data from randomised trials". Lancet. 392 (10145): 387–399. doi:10.1016/S0140-6736(18)31133-4. PMC 6083400. PMID 30017552.
- ^ Bowman L, Mafham M, Wallendszus K, Stevens W, Buck G, Barton J, et al. (October 2018). "Effects of Aspirin for Primary Prevention in Persons with Diabetes Mellitus". The New England Journal of Medicine. 379 (16): 1529–1539. doi:10.1056/NEJMoa1804988. PMID 30146931.
- ^ McNeil JJ, Wolfe R, Woods RL, Tonkin AM, Donnan GA, Nelson MR, et al. (October 2018). "Effect of Aspirin on Cardiovascular Events and Bleeding in the Healthy Elderly". The New England Journal of Medicine. 379 (16): 1509–1518. doi:10.1056/NEJMoa1805819. PMC 6289056. PMID 30221597.
- ^ Woods RL, Polekhina G, Wolfe R, Nelson MR, Ernst ME, Reid CM, et al. (March 2020). "No Modulation of the Effect of Aspirin by Body Weight in Healthy Older Men and Women". Circulation. 141 (13): 1110–1112. doi:10.1161/CIRCULATIONAHA.119.044142. PMC 7286412. PMID 32223674.
- ^ National Guideline Clearinghouse (NGC). "2011 ACCF/AHA/SCAI guideline for percutaneous coronary artery intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions". United States Agency for Healthcare Research and Quality (AHRQ). Archived from the original on 13 August 2012. Retrieved 28 August 2012.
- ^ Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK (August 2001). "Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation" (PDF). The New England Journal of Medicine. 345 (7): 494–502. doi:10.1056/nejmoa010746. PMID 11519503. S2CID 15459216.
- ^ Costa F, Vranckx P, Leonardi S, Moscarella E, Ando G, Calabro P, et al. (May 2015). "Impact of clinical presentation on ischaemic and bleeding outcomes in patients receiving 6- or 24-month duration of dual-antiplatelet therapy after stent implantation: a pre-specified analysis from the PRODIGY (Prolonging Dual-Antiplatelet Treatment After Grading Stent-Induced Intimal Hyperplasia) trial". European Heart Journal. 36 (20): 1242–51. doi:10.1016/s0735-1097(15)61590-x. PMID 25718355.
- ^ Khan SU, Singh M, Valavoor S, Khan MU, Lone AN, Khan MZ, et al. (October 2020). "Dual Antiplatelet Therapy After Percutaneous Coronary Intervention and Drug-Eluting Stents: A Systematic Review and Network Meta-Analysis". Circulation. 142 (15): 1425–1436. doi:10.1161/CIRCULATIONAHA.120.046308. PMC 7547897. PMID 32795096.
- ^ Capodanno D, Alfonso F, Levine GN, Valgimigli M, Angiolillo DJ (December 2018). "ACC/AHA Versus ESC Guidelines on Dual Antiplatelet Therapy: JACC Guideline Comparison". Journal of the American College of Cardiology. 72 (23 Pt A): 2915–2931. doi:10.1016/j.jacc.2018.09.057. PMID 30522654.
- ^ Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, et al. (September 2016). "2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Journal of the American College of Cardiology. 68 (10): 1082–115. doi:10.1016/j.jacc.2016.03.513. PMID 27036918.
- ^ Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, et al. (January 2018). "2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS)". European Heart Journal. 39 (3): 213–260. doi:10.1093/eurheartj/ehx419. PMID 28886622.
- ^ a b Visseren FL, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. (September 2021). "2021 ESC Guidelines on cardiovascular disease prevention in clinical practice". European Heart Journal. 42 (34): 3227–3337. doi:10.1093/eurheartj/ehab484. PMID 34458905.
- ^ Norris JW (September 2005). "Antiplatelet agents in secondary prevention of stroke: a perspective". Stroke. 36 (9): 2034–6. doi:10.1161/01.STR.0000177887.14339.46. PMID 16100022.
- ^ Sleight P, Pouleur H, Zannad F (July 2006). "Benefits, challenges, and registerability of the polypill". European Heart Journal. 27 (14): 1651–6. doi:10.1093/eurheartj/ehi841. PMID 16603580.
- ^ Wang TH, Bhatt DL, Topol EJ (March 2006). "Aspirin and clopidogrel resistance: an emerging clinical entity". European Heart Journal. 27 (6): 647–54. doi:10.1093/eurheartj/ehi684. PMID 16364973.
- ^ Oliveira DC, Silva RF, Silva DJ, Lima VC (September 2010). "Aspirin resistance: fact or fiction?". Arquivos Brasileiros de Cardiologia. 95 (3): e91-4. doi:10.1590/S0066-782X2010001300024. PMID 20944898.
- ^ Topçuoglu MA, Arsava EM, Ay H (February 2011). "Antiplatelet resistance in stroke". Expert Review of Neurotherapeutics. 11 (2): 251–63. doi:10.1586/ern.10.203. PMC 3086673. PMID 21306212.
- ^ Ben-Dor I, Kleiman NS, Lev E (July 2009). "Assessment, mechanisms, and clinical implication of variability in platelet response to aspirin and clopidogrel therapy". The American Journal of Cardiology. 104 (2): 227–33. doi:10.1016/j.amjcard.2009.03.022. PMID 19576352.
- ^
 This article incorporates text from this source, which is in the public domain: "Recommendation: Aspirin Use to Prevent Cardiovascular Disease: Preventive Medication". United States Preventive Services Taskforce. 23 November 2020. Retrieved 5 May 2022.
This article incorporates text from this source, which is in the public domain: "Recommendation: Aspirin Use to Prevent Cardiovascular Disease: Preventive Medication". United States Preventive Services Taskforce. 23 November 2020. Retrieved 5 May 2022.
- ^ Davidson KW, Barry MJ, Mangione CM, Cabana M, Chelmow D, Coker TR, et al. (April 2022). "Aspirin Use to Prevent Cardiovascular Disease: US Preventive Services Task Force Recommendation Statement". JAMA. 327 (16): 1577–1584. doi:10.1001/jama.2022.4983. PMID 35471505.
- ^ Aubrey A, Stone W (26 April 2022). "Older adults shouldn't start a routine of daily aspirin, task force says". NPR.
- ^ a b Cuzick J, Thorat MA, Bosetti C, Brown PH, Burn J, Cook NR, et al. (January 2015). "Estimates of benefits and harms of prophylactic use of aspirin in the general population". Annals of Oncology. 26 (1): 47–57. doi:10.1093/annonc/mdu225. PMC 4269341. PMID 25096604.
- ^ Manzano A, Pérez-Segura P (29 April 2012). "Colorectal cancer chemoprevention: is this the future of colorectal cancer prevention?". TheScientificWorldJournal. 2012: 327341. doi:10.1100/2012/327341. PMC 3353298. PMID 22649288.
- ^ Chan AT, Arber N, Burn J, Chia WK, Elwood P, Hull MA, et al. (February 2012). "Aspirin in the chemoprevention of colorectal neoplasia: an overview". Cancer Prevention Research. 5 (2): 164–78. doi:10.1158/1940-6207.CAPR-11-0391. PMC 3273592. PMID 22084361.
- ^ Thun MJ, Jacobs EJ, Patrono C (April 2012). "The role of aspirin in cancer prevention". Nature Reviews. Clinical Oncology. 9 (5): 259–67. doi:10.1038/nrclinonc.2011.199. PMID 22473097. S2CID 3332999.
- ^ Richman IB, Owens DK (July 2017). "Aspirin for Primary Prevention". The Medical Clinics of North America (Review). 101 (4): 713–724. doi:10.1016/j.mcna.2017.03.004. PMID 28577622.
- ^ Verdoodt F, Friis S, Dehlendorff C, Albieri V, Kjaer SK (February 2016). "Non-steroidal anti-inflammatory drug use and risk of endometrial cancer: A systematic review and meta-analysis of observational studies". Gynecologic Oncology. 140 (2): 352–8. doi:10.1016/j.ygyno.2015.12.009. PMID 26701413.
- ^ Bosetti C, Rosato V, Gallus S, Cuzick J, La Vecchia C (June 2012). "Aspirin and cancer risk: a quantitative review to 2011". Annals of Oncology. 23 (6): 1403–15. doi:10.1093/annonc/mds113. PMID 22517822.
- ^ Sutcliffe P, Connock M, Gurung T, Freeman K, Johnson S, Kandala NB, et al. (September 2013). "Aspirin for prophylactic use in the primary prevention of cardiovascular disease and cancer: a systematic review and overview of reviews". Health Technology Assessment. 17 (43): 1–253. doi:10.3310/hta17430. PMC 4781046. PMID 24074752.
- ^ Kim SE (2014). "The benefit-risk consideration in long-term use of alternate-day, low dose aspirin: focus on colorectal cancer prevention". Annals of Gastroenterology. 27 (1): 87–88. PMC 3959543. PMID 24714632.
- ^ U.S. Preventive Services Task Force (March 2007). "Routine aspirin or nonsteroidal anti-inflammatory drugs for the primary prevention of colorectal cancer: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 146 (5): 361–4. doi:10.7326/0003-4819-146-5-200703060-00008. PMID 17339621.
- ^ Bibbins-Domingo K (June 2016). "Aspirin Use for the Primary Prevention of Cardiovascular Disease and Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement". Annals of Internal Medicine. 164 (12): 836–45. doi:10.7326/m16-0577. PMID 27064677.
- Lay summary in: "Who developed these recommendations?". Annals of Internal Medicine. 21 June 2016.
- ^ Bosetti C, Santucci C, Gallus S, Martinetti M, La Vecchia C (May 2020). "Aspirin and the risk of colorectal and other digestive tract cancers: an updated meta-analysis through 2019". Annals of Oncology. 31 (5): 558–568. doi:10.1016/j.annonc.2020.02.012. hdl:2434/730600. PMID 32272209.
The present comprehensive meta-analysis supports and further quantifies the inverse association between regular aspirin use and the risk of colorectal and other digestive tract cancers, including some rare ones. The favorable effect of aspirin increases with longer duration of use, and, for colorectal cancer, with increasing dose.
- ^ McNeil JJ, Nelson MR, Woods RL, Lockery JE, Wolfe R, Reid CM, et al. (October 2018). "Effect of Aspirin on All-Cause Mortality in the Healthy Elderly". The New England Journal of Medicine. 379 (16): 1519–1528. doi:10.1056/NEJMoa1803955. PMC 6433466. PMID 30221595.
- ^ a b c d e Bartoli F, Cavaleri D, Bachi B, Moretti F, Riboldi I, Crocamo C, et al. (November 2021). "Repurposed drugs as adjunctive treatments for mania and bipolar depression: A meta-review and critical appraisal of meta-analyses of randomized placebo-controlled trials". Journal of Psychiatric Research. 143: 230–238. doi:10.1016/j.jpsychires.2021.09.018. PMID 34509090. S2CID 237485915.
- ^ Dominiak M, Gędek A, Sikorska M, Mierzejewski P, Wojnar M, Antosik-Wójcińska AZ (December 2022). "Acetylsalicylic Acid and Mood Disorders: A Systematic Review". Pharmaceuticals. 16 (1): 67. doi:10.3390/ph16010067. PMC 9861965. PMID 36678565.
- ^ Savitz JB, Teague TK, Misaki M, Macaluso M, Wurfel BE, Meyer M, et al. (January 2018). "Treatment of bipolar depression with minocycline and/or aspirin: an adaptive, 2×2 double-blind, randomized, placebo-controlled, phase IIA clinical trial". Translational Psychiatry. 8 (1): 27. doi:10.1038/s41398-017-0073-7. PMC 5802452. PMID 29362444.
- ^ Bauer IE, Green C, Colpo GD, Teixeira AL, Selvaraj S, Durkin K, et al. (December 2018). "A Double-Blind, Randomized, Placebo-Controlled Study of Aspirin and N-Acetylcysteine as Adjunctive Treatments for Bipolar Depression". The Journal of Clinical Psychiatry. 80 (1). doi:10.4088/JCP.18m12200. PMID 30549489. S2CID 56483705.
- ^ Li H, Li W, Zhang X, Ma XC, Zhang RW (4 February 2021). "Aspirin Use on Incident Dementia and Mild Cognitive Decline: A Systematic Review and Meta-Analysis". Frontiers in Aging Neuroscience. 12: 578071. doi:10.3389/fnagi.2020.578071. PMC 7890199. PMID 33613260.
- ^ Veronese N, Stubbs B, Maggi S, Thompson T, Schofield P, Muller C, et al. (August 2017). "Low-Dose Aspirin Use and Cognitive Function in Older Age: A Systematic Review and Meta-analysis". Journal of the American Geriatrics Society. 65 (8): 1763–1768. doi:10.1111/jgs.14883. PMC 6810633. PMID 28425093.
- ^ Schmidt L, Phelps E, Friedel J, Shokraneh F (August 2019). "Acetylsalicylic acid (aspirin) for schizophrenia". The Cochrane Database of Systematic Reviews. 2019 (8): CD012116. doi:10.1002/14651858.CD012116.pub2. PMC 6699651. PMID 31425623.
- ^ Fond G, Lançon C, Korchia T, Auquier P, Boyer L (2020). "The Role of Inflammation in the Treatment of Schizophrenia". Frontiers in Psychiatry. 11: 160. doi:10.3389/fpsyt.2020.00160. PMC 7093323. PMID 32256401.
- ^ a b National Heart Foundation of Australia (RF/RHD guideline development working group) and the Cardiac Society of Australia and New Zealand (2006). "Diagnosis and management of acute rheumatic fever and rheumatic heart disease in Australia. An evidence-based review" (PDF). National Heart Foundation of Australia. pp. 33–37. Archived from the original (PDF) on 26 July 2008.
- ^ Saxena A, Kumar RK, Gera RP, Radhakrishnan S, Mishra S, Ahmed Z (July 2008). "Consensus guidelines on pediatric acute rheumatic fever and rheumatic heart disease". Indian Pediatrics. 45 (7): 565–73. PMID 18695275.
- ^ Hashkes PJ, Tauber T, Somekh E, Brik R, Barash J, Mukamel M, et al. (September 2003). "Naproxen as an alternative to aspirin for the treatment of arthritis of rheumatic fever: a randomized trial". The Journal of Pediatrics. 143 (3): 399–401. doi:10.1067/S0022-3476(03)00388-3. PMID 14517527.
- ^ Rowley AH, Shulman ST (February 2010). "Pathogenesis and management of Kawasaki disease". Expert Review of Anti-Infective Therapy. 8 (2): 197–203. doi:10.1586/eri.09.109. PMC 2845298. PMID 20109049.
- ^ Baumer JH, Love SJ, Gupta A, Haines LC, Maconochie I, Dua JS (October 2006). "Salicylate for the treatment of Kawasaki disease in children". The Cochrane Database of Systematic Reviews. 2010 (4): CD004175. doi:10.1002/14651858.CD004175.pub2. PMC 8765111. PMID 17054199.
- ^ Duley L, Meher S, Hunter KE, Seidler AL, Askie LM (October 2019). "Antiplatelet agents for preventing pre-eclampsia and its complications". The Cochrane Database of Systematic Reviews. 2019 (10). doi:10.1002/14651858.CD004659.pub3. PMC 6820858. PMID 31684684.
- ^ Roberge S, Villa P, Nicolaides K, Giguère Y, Vainio M, Bakthi A, et al. (2012). "Early administration of low-dose aspirin for the prevention of preterm and term preeclampsia: a systematic review and meta-analysis". Fetal Diagnosis and Therapy. 31 (3): 141–6. doi:10.1159/000336662. PMID 22441437. S2CID 26372982.
- ^ Roberge S, Nicolaides K, Demers S, Hyett J, Chaillet N, Bujold E (February 2017). "The role of aspirin dose on the prevention of preeclampsia and fetal growth restriction: systematic review and meta-analysis". American Journal of Obstetrics and Gynecology. 216 (2): 110–120.e6. doi:10.1016/j.ajog.2016.09.076. PMID 27640943. S2CID 3079979.
- ^ Szabó B, Németh K, Mészáros K, Krokker L, Likó I, Saskői E, et al. (5 September 2022). "Aspirin Mediates Its Antitumoral Effect Through Inhibiting PTTG1 in Pituitary Adenoma". The Journal of Clinical Endocrinology and Metabolism. 107 (11): 3066–3079. doi:10.1210/clinem/dgac496. PMC 9681612. PMID 36059148.
- ^ Dorsch MP, Lee JS, Lynch DR, Dunn SP, Rodgers JE, Schwartz T, et al. (May 2007). "Aspirin resistance in patients with stable coronary artery disease with and without a history of myocardial infarction". The Annals of Pharmacotherapy. 41 (5): 737–41. doi:10.1345/aph.1H621. PMID 17456544. S2CID 22245507.
- ^ a b Krasopoulos G, Brister SJ, Beattie WS, Buchanan MR (January 2008). "Aspirin "resistance" and risk of cardiovascular morbidity: systematic review and meta-analysis". BMJ. 336 (7637): 195–8. doi:10.1136/bmj.39430.529549.BE. PMC 2213873. PMID 18202034.
- ^ Pignatelli P, Di Santo S, Barillà F, Gaudio C, Violi F (October 2008). "Multiple anti-atherosclerotic treatments impair aspirin compliance: effects on aspirin resistance". Journal of Thrombosis and Haemostasis. 6 (10): 1832–4. doi:10.1111/j.1538-7836.2008.03122.x. PMID 18680540. S2CID 1776526.
- ^ Grosser T, Fries S, Lawson JA, Kapoor SC, Grant GR, FitzGerald GA (January 2013). "Drug resistance and pseudoresistance: an unintended consequence of enteric coating aspirin". Circulation. 127 (3): 377–85. doi:10.1161/CIRCULATIONAHA.112.117283. PMC 3552520. PMID 23212718.
- Lay summary in: Thomas K (4 December 2012). "Study Raises Questions on Coating of Aspirin". The New York Times.
- ^ Li J, Song M, Jian Z, Guo W, Chen G, Jiang G, et al. (2014). "Laboratory aspirin resistance and the risk of major adverse cardiovascular events in patients with coronary heart disease on confirmed aspirin adherence". Journal of Atherosclerosis and Thrombosis. 21 (3): 239–47. doi:10.5551/jat.19521. PMID 24201035.
- ^ Sofi F, Marcucci R, Gori AM, Abbate R, Gensini GF (August 2008). "Residual platelet reactivity on aspirin therapy and recurrent cardiovascular events--a meta-analysis". International Journal of Cardiology. 128 (2): 166–71. doi:10.1016/j.ijcard.2007.12.010. hdl:2158/323452. PMID 18242733.
- ^ Shim EJ, Ryu CW, Park S, Lee HN, Shin HS, Kim SB (October 2018). "Relationship between adverse events and antiplatelet drug resistance in neurovascular intervention: a meta-analysis". Journal of NeuroInterventional Surgery. 10 (10): 942–948. doi:10.1136/neurintsurg-2017-013632. PMID 29352056. S2CID 38147668.
- ^ Fiolaki A, Katsanos AH, Kyritsis AP, Papadaki S, Kosmidou M, Moschonas IC, et al. (May 2017). "High on treatment platelet reactivity to aspirin and clopidogrel in ischemic stroke: A systematic review and meta-analysis". Journal of the Neurological Sciences. 376: 112–116. doi:10.1016/j.jns.2017.03.010. PMID 28431593. S2CID 3485236.
- ^ Snoep JD, Hovens MM, Eikenboom JC, van der Bom JG, Huisman MV (13 August 2007). "Association of laboratory-defined aspirin resistance with a higher risk of recurrent cardiovascular events: a systematic review and meta-analysis". Archives of Internal Medicine. 167 (15): 1593–9. doi:10.1001/archinte.167.15.1593. PMID 17698681.
- ^ a b van Oosterom N, Barras M, Bird R, Nusem I, Cottrell N (December 2020). "A Narrative Review of Aspirin Resistance in VTE Prophylaxis for Orthopaedic Surgery". Drugs. 80 (18): 1889–1899. doi:10.1007/s40265-020-01413-w. PMID 33037568. S2CID 222234431.
- ^ "Invention of the safety cap". digitaldukemed.mc.duke.edu. Archived from the original on 4 March 2016. Retrieved 4 September 2015.
- ^ a b British National Formulary (45 ed.). British Medical Journal and Royal Pharmaceutical Society of Great Britain. 2003.
- ^ "Aspirin monograph: dosages, etc". Medscape.com. Retrieved 11 May 2011.
- ^ US Preventive Services Task Force (March 2009). "Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 150 (6): 396–404. doi:10.7326/0003-4819-150-6-200903170-00008. PMID 19293072.
- ^ a b "Aspirin: more evidence that low dose is all that is needed". Medscape. Medscape CME. Retrieved 11 May 2011.
- ^ Berger JS, Brown DL, Burke GL, Oberman A, Kostis JB, Langer RD, et al. (March 2009). "Aspirin Use, Dose, and Clinical Outcomes in Postmenopausal Women With Stable Cardiovascular Disease". Circulation: Cardiovascular Quality and Outcomes. 2 (2): 78–87. doi:10.1161/circoutcomes.108.791269. ISSN 1941-7713. PMC 2801891. PMID 20031819.
- ^ Sacristán JA (August 2021). "Aspirin Dosing in Cardiovascular Disease". New England Journal of Medicine. 385 (8): 764–765. doi:10.1056/nejmc2110476. ISSN 0028-4793. PMID 34407352. S2CID 237214969.
- ^ British National Formulary for Children. British Medical Journal and Royal Pharmaceutical Society. 2006.
- ^ a b
 This article incorporates text from this source, which is in the public domain: "FDA Warns that Using a Type of Pain and Fever Medication in Second Half of Pregnancy Could Lead to Complications". U.S. Food and Drug Administration (FDA) (Press release). 15 October 2020. Retrieved 15 October 2020.
This article incorporates text from this source, which is in the public domain: "FDA Warns that Using a Type of Pain and Fever Medication in Second Half of Pregnancy Could Lead to Complications". U.S. Food and Drug Administration (FDA) (Press release). 15 October 2020. Retrieved 15 October 2020.
- ^ a b c
 This article incorporates text from this source, which is in the public domain: "NSAIDs may cause rare kidney problems in unborn babies". U.S. Food and Drug Administration. 21 July 2017. Retrieved 15 October 2020.
This article incorporates text from this source, which is in the public domain: "NSAIDs may cause rare kidney problems in unborn babies". U.S. Food and Drug Administration. 21 July 2017. Retrieved 15 October 2020.
- ^ a b c d e "Aspirin information from Drugs.com". Drugs.com. Archived from the original on 9 May 2008. Retrieved 8 May 2008.
- ^ a b c "Oral Aspirin information". First DataBank. Archived from the original on 18 September 2000. Retrieved 8 May 2008.
- ^ Raithel M, Baenkler HW, Naegel A, Buchwald F, Schultis HW, Backhaus B, et al. (September 2005). "Significance of salicylate intolerance in diseases of the lower gastrointestinal tract" (PDF). Journal of Physiology and Pharmacology. 56 (Suppl 5): 89–102. PMID 16247191. Archived (PDF) from the original on 9 April 2011.
- ^ Senna GE, Andri G, Dama AR, Mezzelani P, Andri L (1995). "Tolerability of imidazole salycilate in aspirin-sensitive patients". Allergy Proceedings. 16 (5): 251–254. doi:10.2500/108854195778702675. PMID 8566739.
- ^ a b "PDR guide to over the counter (OTC) drugs". Archived from the original on 10 April 2008. Retrieved 28 April 2008.
- ^ Livingstone FB (1985). Frequencies of hemoglobin variants: thalassemia, the glucose-6-phosphate dehydrogenase deficiency, G6PD variants, and ovalocytosis in human populations. Oxford University Press. ISBN 978-0-19-503634-3.
- ^ "Dengue and dengue hemorrhagic fever: information for health care practitioners". Archived from the original on 17 March 2008. Retrieved 28 April 2008.
- ^ Zhang Y, Neogi T, Chen C, Chaisson C, Hunter DJ, Choi H (February 2014). "Low-dose aspirin use and recurrent gout attacks". Annals of the Rheumatic Diseases. 73 (2): 385–390. doi:10.1136/annrheumdis-2012-202589. PMC 3902644. PMID 23345599.
- ^ Polkinghorne KR, Wetmore JB, Thao LT, Wolfe R, Woods RL, Ernst ME, et al. (December 2022). "Effect of Aspirin on CKD Progression in Older Adults: Secondary Analysis From the ASPREE Randomized Clinical Trial". American Journal of Kidney Diseases. 80 (6): 810–813. doi:10.1053/j.ajkd.2022.02.019. PMC 9562592. PMID 35430328.
- ^ Mann JF, Joseph P, Gao P, Pais P, Tyrwhitt J, Xavier D, et al. (February 2023). "Effects of aspirin on cardiovascular outcomes in patients with chronic kidney disease". Kidney International. 103 (2): 403–410. doi:10.1016/j.kint.2022.09.023. PMID 36341885. S2CID 253194139.
- ^ a b Macdonald S (November 2002). "Aspirin use to be banned in under 16 year olds". BMJ. 325 (7371): 988c–988. doi:10.1136/bmj.325.7371.988/c. PMC 1169585. PMID 12411346.
- ^ a b c Sørensen HT, Mellemkjaer L, Blot WJ, Nielsen GL, Steffensen FH, McLaughlin JK, et al. (September 2000). "Risk of upper gastrointestinal bleeding associated with use of low-dose aspirin". The American Journal of Gastroenterology. 95 (9): 2218–2224. doi:10.1016/s0002-9270(00)01040-6. PMID 11007221.
- ^ Kedir HM, Sisay EA, Abiye AA (2021). "Enteric-Coated Aspirin and the Risk of Gastrointestinal Side Effects: A Systematic Review". International Journal of General Medicine. 14: 4757–4763. doi:10.2147/ijgm.s326929. PMC 8403009. PMID 34466020.
- ^ Torborg L (4 December 2018). "Mayo Clinic Q and A: Coated aspirin may not be as effective at reducing blood clot risk". Mayo Clinic News Network.
- ^ Cox D, Maree AO, Dooley M, Conroy R, Byrne MF, Fitzgerald DJ (August 2006). "Effect of enteric coating on antiplatelet activity of low-dose aspirin in healthy volunteers". Stroke. 37 (8): 2153–2158. doi:10.1161/01.STR.0000231683.43347.ec. PMID 16794200. S2CID 8034371.
- ^ Delaney JA, Opatrny L, Brophy JM, Suissa S (August 2007). "Drug drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding". CMAJ. 177 (4): 347–351. doi:10.1503/cmaj.070186. PMC 1942107. PMID 17698822.
- ^ Wallace JL (October 2008). "Prostaglandins, NSAIDs, and gastric mucosal protection: why doesn't the stomach digest itself?". Physiological Reviews. 88 (4): 1547–65. doi:10.1152/physrev.00004.2008. PMID 18923189. S2CID 448875.
- ^ Rostom A, Muir K, Dubé C, Jolicoeur E, Boucher M, Joyce J, et al. (July 2007). "Gastrointestinal safety of cyclooxygenase-2 inhibitors: a Cochrane Collaboration systematic review". Clinical Gastroenterology and Hepatology. 5 (7): 818–28, 828.e1-5, quiz 768. doi:10.1016/j.cgh.2007.03.011. PMID 17556027.
- ^ Clerici B, Cattaneo M (March 2023). "Pharmacological Efficacy and Gastrointestinal Safety of Different Aspirin Formulations for Cardiovascular Prevention: A Narrative Review". Journal of Cardiovascular Development and Disease. 10 (4): 137. doi:10.3390/jcdd10040137. PMC 10145431. PMID 37103016.
- ^ "General chemistry online: FAQ: Acids and bases: What is the buffer system in buffered aspirin?". Antoine.frostburg.edu. Archived from the original on 14 April 2011. Retrieved 11 May 2011.
- ^ Davison C, Smith BW, Smith PK (August 1962). "Effects of buffered and unbuffered acetylsalicylic acid upon the gastric acidity of normal human subjects". Journal of Pharmaceutical Sciences. 51 (8): 759–763. doi:10.1002/jps.2600510813. PMID 13883982.
- ^ Dammann HG, Saleki M, Torz M, Schulz HU, Krupp S, Schürer M, et al. (February 2004). "Effects of buffered and plain acetylsalicylic acid formulations with and without ascorbic acid on gastric mucosa in healthy subjects". Alimentary Pharmacology & Therapeutics. 19 (3): 367–74. doi:10.1111/j.1365-2036.2004.01742.x. PMID 14984384. S2CID 22688422.
- ^ Konturek PC, Kania J, Hahn EG, Konturek JW (November 2006). "Ascorbic acid attenuates aspirin-induced gastric damage: role of inducible nitric oxide synthase". Journal of Physiology and Pharmacology. 57 (Suppl 5): 125–36. PMID 17218764.
- ^ Hayreh SS (July 2014). "Ocular vascular occlusive disorders: natural history of visual outcome". Progress in Retinal and Eye Research. 41: 1–25. doi:10.1016/j.preteyeres.2014.04.001. PMC 4073304. PMID 24769221.
- ^ Ageno W, Beyer-Westendorf J, Garcia DA, Lazo-Langner A, McBane RD, Paciaroni M (January 2016). "Guidance for the management of venous thrombosis in unusual sites". Journal of Thrombosis and Thrombolysis. 41 (1): 129–43. doi:10.1007/s11239-015-1308-1. PMC 4715841. PMID 26780742.
- ^ Guitton MJ, Caston J, Ruel J, Johnson RM, Pujol R, Puel JL (May 2003). "Salicylate induces tinnitus through activation of cochlear NMDA receptors". The Journal of Neuroscience. 23 (9): 3944–52. doi:10.1523/JNEUROSCI.23-09-03944.2003. PMC 6742173. PMID 12736364.
- ^ a b Belay ED, Bresee JS, Holman RC, Khan AS, Shahriari A, Schonberger LB (May 1999). "Reye's syndrome in the United States from 1981 through 1997". The New England Journal of Medicine. 340 (18): 1377–82. doi:10.1056/NEJM199905063401801. PMID 10228187.
- ^ "Reye's syndrome". Health A to Z. National Health Service. 14 September 2023. Retrieved 24 August 2024.
- ^ "Are You Sensitive to Aspirin? Here are Some Reasons Why". Health Essentials from Cleveland Clinic. 5 February 2015. Archived from the original on 25 October 2020. Retrieved 5 March 2020.
- ^ a b c Doña I, Barrionuevo E, Salas M, Laguna JJ, Agúndez J, García-Martín E, et al. (November 2018). "NSAIDs-hypersensitivity often induces a blended reaction pattern involving multiple organs". Scientific Reports. 8 (1): 16710. Bibcode:2018NatSR...816710D. doi:10.1038/s41598-018-34668-1. PMC 6232098. PMID 30420763.
- ^ a b Kowalski ML, Agache I, Bavbek S, Bakirtas A, Blanca M, Bochenek G, et al. (January 2019). "Diagnosis and management of NSAID-Exacerbated Respiratory Disease (N-ERD)-a EAACI position paper". Allergy. 74 (1): 28–39. doi:10.1111/all.13599. PMID 30216468. S2CID 52276808.
- ^ Sánchez-Borges M, Capriles-Hulett A (January 2000). "Atopy is a risk factor for non-steroidal anti-inflammatory drug sensitivity". Annals of Allergy, Asthma & Immunology. 84 (1): 101–6. doi:10.1016/S1081-1206(10)62748-2. PMID 10674573.
- ^ Stadelmann WK, Digenis AG, Tobin GR (August 1998). "Impediments to wound healing". American Journal of Surgery. 176 (2A Suppl): 39S–47S. doi:10.1016/S0002-9610(98)00184-6. PMID 9777971.
- ^ Layton AM, Ibbotson SH, Davies JA, Goodfield MJ (July 1994). "Randomised trial of oral aspirin for chronic venous leg ulcers". Lancet. 344 (8916): 164–5. doi:10.1016/s0140-6736(94)92759-6. PMID 7912767. S2CID 912169.
- ^ del Río Solá ML, Antonio J, Fajardo G, Vaquero Puerta C (July 2012). "Influence of aspirin therapy in the ulcer associated with chronic venous insufficiency". Annals of Vascular Surgery. 26 (5): 620–9. doi:10.1016/j.avsg.2011.02.051. hdl:10324/2904. PMID 22437068.
- ^ de Oliveira Carvalho PE, Magolbo NG, De Aquino RF, Weller CD, et al. (Cochrane Wounds Group) (February 2016). "Oral aspirin for treating venous leg ulcers". The Cochrane Database of Systematic Reviews. 2016 (2): CD009432. doi:10.1002/14651858.CD009432.pub2. PMC 8627253. PMID 26889740.
- ^ Jull A, Wadham A, Bullen C, Parag V, Kerse N, Waters J (November 2017). "Low dose aspirin as adjuvant treatment for venous leg ulceration: pragmatic, randomised, double blind, placebo controlled trial (Aspirin4VLU)". BMJ. 359: j5157. doi:10.1136/bmj.j5157. PMC 5701114. PMID 29175902.
- ^ Tilbrook H, Clark L, Cook L, Bland M, Buckley H, Chetter I, et al. (October 2018). "AVURT: aspirin versus placebo for the treatment of venous leg ulcers - a Phase II pilot randomised controlled trial". Health Technology Assessment. 22 (55): 1–138. doi:10.3310/hta22550. PMC 6204573. PMID 30325305.
- ^ Berges-Gimeno MP, Stevenson DD (June 2004). "Nonsteroidal anti-inflammatory drug-induced reactions and desensitization". The Journal of Asthma. 41 (4): 375–84. doi:10.1081/JAS-120037650. PMID 15281324. S2CID 29909460.
- ^ Vernooij MW, Haag MD, van der Lugt A, Hofman A, Krestin GP, Stricker BH, et al. (June 2009). "Use of antithrombotic drugs and the presence of cerebral microbleeds: the Rotterdam Scan Study". Archives of Neurology. 66 (6): 714–20. doi:10.1001/archneurol.2009.42. PMID 19364926.
- ^ Gorelick PB (June 2009). "Cerebral microbleeds: evidence of heightened risk associated with aspirin use". Archives of Neurology. 66 (6): 691–3. doi:10.1001/archneurol.2009.85. PMID 19506128.
- ^ a b He J, Whelton PK, Vu B, Klag MJ (December 1998). "Aspirin and risk of hemorrhagic stroke: a meta-analysis of randomized controlled trials". JAMA. 280 (22): 1930–5. doi:10.1001/jama.280.22.1930. PMID 9851479. S2CID 22997730.
- ^ Saloheimo P, Ahonen M, Juvela S, Pyhtinen J, Savolainen ER, Hillbom M (January 2006). "Regular aspirin-use preceding the onset of primary intracerebral hemorrhage is an independent predictor for death". Stroke. 37 (1): 129–33. doi:10.1161/01.STR.0000196991.03618.31. PMID 16322483.
- ^ Medical knowledge self-assessment program for students 4, By American College of Physicians, Clerkship Directors in Internal Medicine, Nephrology 227, Item 29
- ^ Biondi-Zoccai GG, Lotrionte M, Agostoni P, Abbate A, Fusaro M, Burzotta F, et al. (November 2006). "A systematic review and meta-analysis on the hazards of discontinuing or not adhering to aspirin among 50,279 patients at risk for coronary artery disease". European Heart Journal. 27 (22): 2667–2674. doi:10.1093/eurheartj/ehl334. PMID 17053008.
- ^ a b "FDA strengthens warning of heart attack and stroke risk for non-steroidal anti-inflammatory drugs". U.S. Food and Drug Administration (FDA). 9 July 2015. Archived from the original on 11 July 2015. Retrieved 9 July 2015.
- ^ Kreplick LW (2001). "Salicylate toxicity in emergency medicine". Medscape. Archived from the original on 31 August 2012.
- ^ Gaudreault P, Temple AR, Lovejoy FH (October 1982). "The relative severity of acute versus chronic salicylate poisoning in children: a clinical comparison". Pediatrics. 70 (4): 566–9. doi:10.1542/peds.70.4.566. PMID 7122154. S2CID 12738659. (primary source)
- ^ Marx J (2006). Rosen's emergency medicine: concepts and clinical practice. Mosby/Elsevier. p. 2242. ISBN 978-0-323-02845-5.
- ^ Morra P, Bartle WR, Walker SE, Lee SN, Bowles SK, Reeves RA (September 1996). "Serum concentrations of salicylic acid following topically applied salicylate derivatives". The Annals of Pharmacotherapy. 30 (9): 935–40. doi:10.1177/106002809603000903. PMID 8876850. S2CID 9843820.
- ^ Baselt R (2011). Disposition of toxic drugs and chemicals in man (9th ed.). Seal Beach, California: Biomedical Publications. pp. 20–23. ISBN 978-0-9626523-8-7.
- ^ a b Alqahtani Z, Jamali F (2018). "Clinical Outcomes of Aspirin Interaction with Other Non-Steroidal Anti-Inflammatory Drugs: A Systematic Review". Journal of Pharmacy & Pharmaceutical Sciences. 21 (1s): 48s–73s. doi:10.18433/jpps29854. PMID 29891025. S2CID 48361086.
- ^ Gladding PA, Webster MW, Farrell HB, Zeng IS, Park R, Ruijne N (April 2008). "The antiplatelet effect of six non-steroidal anti-inflammatory drugs and their pharmacodynamic interaction with aspirin in healthy volunteers". The American Journal of Cardiology. 101 (7): 1060–1063. doi:10.1016/j.amjcard.2007.11.054. PMID 18359332.
- ^ Baxter K, Preston CL (eds.). "Aspirin and Spironolactone". MedicinesComplete: Stockley's Drug Interactions. Royal Pharmaceutical Society.
- ^ Hollifield JW (August 1976). "Failure of aspirin to antagonize the antihypertensive effect of spironolactone in low-renin hypertension". Southern Medical Journal. 69 (8): 1034–6. doi:10.1097/00007611-197608000-00022. PMID 785608.
- ^ Katzung BG (1998). Basic and clinical pharmacology. McGraw-Hill. p. 584. ISBN 978-0-8385-0565-6.
- ^ Loh HS, Watters K, Wilson CW (1 November 1973). "The effects of aspirin on the metabolic availability of ascorbic acid in human beings". Journal of Clinical Pharmacology. 13 (11): 480–486. doi:10.1002/j.1552-4604.1973.tb00203.x. PMID 4490672.
- ^ Basu TK (1982). "Vitamin C-aspirin interactions". International Journal for Vitamin and Nutrition Research. Supplement. 23: 83–90. PMID 6811490.
- ^ Ioannides C, Stone AN, Breacker PJ, Basu TK (December 1982). "Impairment of absorption of ascorbic acid following ingestion of aspirin in guinea pigs". Biochemical Pharmacology. 31 (24): 4035–4038. doi:10.1016/0006-2952(82)90652-9. PMID 6818974.
- ^ "Randomised Trial of Intravenous Streptokinase, Oral Aspirin, Both, or Neither Among 17,187 Cases of Suspected Acute Myocardial Infarction: Isis-2". The Lancet. 332 (8607): 349–360. August 1988. doi:10.1016/s0140-6736(88)92833-4. ISSN 0140-6736. PMID 2899772. S2CID 21071664.
- ^ Lewis HD, Davis JW, Archibald DG, Steinke WE, Smitherman TC, Doherty JE, et al. (August 1983). "Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina. Results of a Veterans Administration Cooperative Study". New England Journal of Medicine. 309 (7): 396–403. doi:10.1056/NEJM198308183090703. ISSN 0028-4793. PMID 6135989.
- ^ Di Bella S, Luzzati R, Principe L, Zerbato V, Meroni E, Giuffrè M, et al. (25 January 2022). "Aspirin and Infection: A Narrative Review". Biomedicines. 10 (2): 263. doi:10.3390/biomedicines10020263. ISSN 2227-9059. PMC 8868581. PMID 35203473.
- ^ Cao Y, Tan A (September 2020). "Aspirin might reduce the incidence of breast cancer: An updated meta-analysis of 38 observational studies". Medicine. 99 (38): e21917. doi:10.1097/md.0000000000021917. PMC 7505405. PMID 32957311.
- ^ Cook NR, Lee IM, Gaziano JM, Gordon D, Ridker PM, Manson JE, et al. (July 2005). "Low-dose aspirin in the primary prevention of cancer: the Women's Health Study: a randomized controlled trial". JAMA. 294 (1): 47–55. doi:10.1001/jama.294.1.47. PMID 15998890.
- ^ "Aspirin Water Helps Plants". cybercemetery.unt.edu.
- ^ "Gardens: drug therapy for plants | Gardening advice". The Guardian. 31 January 2016.
- ^ "Priming Plant Defenses with Aspirin-like Compound : USDA ARS". www.ars.usda.gov.
- ^ a b c Edwards SH. "Nonsteroidal Anti-inflammatory Drugs: Aspirin". Merck Veterinary Manual. Archived from the original on 18 December 2016. Retrieved 20 January 2018.
- ^ a b "Analgesics (toxicity)". Merck. Archived from the original on 11 April 2015. Retrieved 19 January 2018.
- ^ Lappin MR, ed. (2001). Feline internal medicine secrets. Philadelphia: Hanley & Belfus. p. 160. ISBN 978-1-56053-461-7.
- ^ "Plants poisonous to livestock". Cornell University Department of Animal Science. Archived from the original on 16 August 2015. Retrieved 3 March 2016.
Further reading
[edit]- Desborough MJ, Keeling DM (June 2017). "The aspirin story - from willow to wonder drug". British Journal of Haematology. 177 (5): 674–683. doi:10.1111/bjh.14520. PMID 28106908. S2CID 46794541.
- McTavish JR (1987). "What's in a name? Aspirin and the American Medical Association". Bulletin of the History of Medicine. 61 (3): 343–66. JSTOR 44442097. PMID 3311247.
- Ling G (2005). "Aspirin". How Products Are Made. Vol. 1. Thomson Gale.
- Diarmuid Jeffreys (2004). Aspirin: the Remarkable Story of a Wonder Drug. Bloomsbury.
External links
[edit] Media related to Aspirin at Wikimedia Commons
Media related to Aspirin at Wikimedia Commons
- Aspirin
- 1897 in Germany
- 1897 in science
- Acetate esters
- Acetylsalicylic acids
- Antiplatelet drugs
- Drugs developed by Bayer
- Brands that became generic
- Chemical substances for emergency medicine
- Commercialization of traditional medicines
- Covalent inhibitors
- Equine medications
- German inventions
- Hepatotoxins
- Nonsteroidal anti-inflammatory drugs
- Salicylic acids
- Salicylyl esters
- World Health Organization essential medicines


