Myeloperoxidase
| Myeloperoxidase | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||
| EC no. | 1.11.2.2 | ||||||||
| Databases | |||||||||
| IntEnz | IntEnz view | ||||||||
| BRENDA | BRENDA entry | ||||||||
| ExPASy | NiceZyme view | ||||||||
| KEGG | KEGG entry | ||||||||
| MetaCyc | metabolic pathway | ||||||||
| PRIAM | profile | ||||||||
| PDB structures | RCSB PDB PDBe PDBsum | ||||||||
| |||||||||
Myeloperoxidase (MPO) is a peroxidase enzyme that in humans is encoded by the MPO gene on chromosome 17.[5] MPO is most abundantly expressed in neutrophils (a subtype of white blood cells), and produces hypohalous acids to carry out their antimicrobial activity, including hypochlorous acid, the sodium salt of which is the chemical in bleach.[5][6] It is a lysosomal protein stored in azurophilic granules of the neutrophil and released into the extracellular space during degranulation.[7] Neutrophil myeloperoxidase has a heme pigment, which causes its green color in secretions rich in neutrophils, such as mucus and sputum.[8] The green color contributed to its outdated name verdoperoxidase.
Myeloperoxidase is found in many different organisms including mammals, birds, fish, reptiles, and amphibians.[citation needed] Myeloperoxidase deficiency is a well-documented disease among humans resulting in impaired immune function.[9]
Function
[edit]MPO is a member of the XPO subfamily of peroxidases and produces hypochlorous acid (HOCl) from hydrogen peroxide (H2O2) and chloride anion (Cl−) (or hypobromous acid if Br- is present) during the neutrophil's respiratory burst. It requires heme as a cofactor. Furthermore, it oxidizes tyrosine to tyrosyl radical using hydrogen peroxide as an oxidizing agent.[10][11]
However, this hypochlorous acid may also cause oxidative damage in host tissue. Moreover, MPO oxidation of apoA-I reduces HDL-mediated inhibition of apoptosis and inflammation.[12] In addition, MPO mediates protein nitrosylation and the formation of 3-chlorotyrosine and dityrosine crosslinks.[10]
Myeloperoxidase is the first and so far only[needs update] human enzyme known to break down carbon nanotubes, allaying a concern among clinicians that using nanotubes for targeted delivery of medicines would lead to an unhealthy buildup of nanotubes in tissues.[13]
Role in innate immunity
[edit]Neutrophils use myeloperoxidase to produce the substances needed for their respiratory burst.[14] Hypochlorous acid and tyrosyl radical are cytotoxic, so they are used by the neutrophil to kill bacteria and certain types of fungi.[14][15][16]
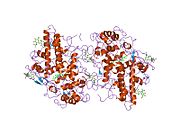
Structure
[edit]The 150-kDa MPO protein is a cationic heterotetramer consisting of two 15-kDa light chains and two variable-weight glycosylated heavy chains bound to a prosthetic heme group complex with calcium ions, arranged as a homodimer of heterodimers. Both are proteolytically generated from the precursor peptide encoded by the MPO gene.[17][10][18][19] The light chains are glycosylated and contain the modified iron protoporphyrin IX active site. Together, the light and heavy chains form two identical 73-kDa monomers connected by a cystine bridge at Cys153. The protein forms a deep crevice which holds the heme group at the bottom, as well as a hydrophobic pocket at the entrance to the distal heme cavity which carries out its catalytic activity.[19]
Variation in glycosylation and the identity of the heavy chain lead to variations in molecular weight within the 135-200 kDa range.[20][17] In mice, three isoforms exist, differing only by the heavy chain.[10]
One of the ligands is the carbonyl group of Asp 96. Calcium-binding is important for structure of the active site because of Asp 96's close proximity to the catalytic His95 side chain.[21]
Reaction mechanism
[edit]The central heme group acts as the active site. The reaction starts when hydrogen peroxide donates an oxygen to the heme group, converting it to an activated form called "Compound I". This compound then oxidizes the chloride ions to form the hypochlorous acid and Compound II, which can be reduced back down to its original heme state.[how?] This cycle continues for as long as the immune system requires.[citation needed]
Clinical significance
[edit]Myeloperoxidase deficiency
[edit]Myeloperoxidase deficiency is a hereditary deficiency of the enzyme, which causes a mild immune deficiency against certain pathogens.[9][14] People with myeloperoxidase deficiency are most at risk of infection by Candida species, which are pathogenic fungi. The most common species found in humans is Candida albicans. There may be an increased risk of certain other infections, such as with Klebsiella pneumoniae, but recurrent candidiasis is the only common clinical consequence, if the patient is noticeably affected at all.[14]
Vasculitis
[edit]Antibodies against MPO have been implicated in various types of vasculitis, most prominently three clinically and pathologically recognized forms: granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA); and eosinophilic granulomatosis with polyangiitis (EGPA). Antibodies are also known as anti-neutrophil cytoplasmic antibodies (ANCAs), though ANCAs have also been detected in staining of the perinuclear region.[22]
Atherosclerosis and heart disease
[edit]Myeloperoxidase is known to contribute to atherosclerosis and diseases related to it, including coronary artery disease. MPO oxidizes LDL cholesterol, and as a result, the LDL receptor in liver cells becomes unable to bind to LDL and remove it from the blood stream. However, in its oxidized state, LDL can still contribute to foam cell formation and other atherosclerotic processes. Thus, elevated levels of MPO are a risk factor for atherosclerosis.[23]
Medical tests
[edit]This section needs to be updated. (January 2025) |
An initial 2003 study suggested that MPO could serve as a sensitive predictor for myocardial infarction in patients presenting with chest pain.[24] Since then, there have been over 100 published studies documenting the utility of MPO testing. The 2010 Heslop et al. study reported that measuring both MPO and CRP (C-reactive protein; a general and cardiac-related marker of inflammation) provided added benefit for risk prediction than just measuring CRP alone.[25]
Immunohistochemical staining for myeloperoxidase used to be administered in the diagnosis of acute myeloid leukemia to demonstrate that the leukemic cells were derived from the myeloid lineage. Myeloperoxidase staining is still important in the diagnosis of myeloid sarcoma, contrasting with the negative staining of lymphomas, which can otherwise have a similar appearance.[26] In the case of screening patients for vasculitis, flow cytometric assays have demonstrated comparable sensitivity to immunofluorescence tests, with the additional benefit of simultaneous detection of multiple autoantibodies relevant to vasculitis. Nonetheless, this method still requires further testing.[27]
Inhibitors of MPO
[edit]Azide has been used traditionally as an MPO inhibitor, but 4-aminobenzoic acid hydrazide (4-ABH) is a more specific inhibitor of MPO.[28]
See also
[edit]References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000005381 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000009350 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b "Entrez Gene: Myeloperoxidase".
- ^ Klebanoff SJ (May 2005). "Myeloperoxidase: friend and foe". Journal of Leukocyte Biology. 77 (5): 598–625. doi:10.1189/jlb.1204697. PMID 15689384. S2CID 12489688.
- ^ Kinkade JM, Pember SO, Barnes KC, Shapira R, Spitznagel JK, Martin LE (Jul 1983). "Differential distribution of distinct forms of myeloperoxidase in different azurophilic granule subpopulations from human neutrophils". Biochemical and Biophysical Research Communications. 114 (1): 296–303. doi:10.1016/0006-291x(83)91627-3. PMID 6192815.
- ^ Le T, Bhushan V, Sochat M, Damisch K, Abrams J, Kallianos K, Boqambar H, Qiu, C, Coleman C (2021). First Aid for the USMLE Step 1 (2021 ed.). New York: McGraw Hill. p. 109. ISBN 9781260467529.
- ^ a b Kutter D, Devaquet P, Vanderstocken G, Paulus JM, Marchal V, Gothot A (2000). "Consequences of total and subtotal myeloperoxidase deficiency: risk or benefit ?". Acta Haematologica. 104 (1): 10–5. doi:10.1159/000041062. PMID 11111115. S2CID 36776058.
- ^ a b c d "Mouse MPO EasyTestTM ELISA Kit" (PDF). Archived from the original (PDF) on 2016-03-03. Retrieved 2015-08-06.
- ^ Heinecke JW, Li W, Francis GA, Goldstein JA (Jun 1993). "Tyrosyl radical generated by myeloperoxidase catalyzes the oxidative cross-linking of proteins". The Journal of Clinical Investigation. 91 (6): 2866–72. doi:10.1172/JCI116531. PMC 443356. PMID 8390491.
- ^ Shao B, Oda MN, Oram JF, Heinecke JW (Mar 2010). "Myeloperoxidase: an oxidative pathway for generating dysfunctional high-density lipoprotein". Chemical Research in Toxicology. 23 (3): 447–54. doi:10.1021/tx9003775. PMC 2838938. PMID 20043647.
- ^ Kagan VE, Konduru NV, Feng W, Allen BL, Conroy J, Volkov Y, Vlasova II, Belikova NA, Yanamala N, Kapralov A, Tyurina YY, Shi J, Kisin ER, Murray AR, Franks J, Stolz D, Gou P, Klein-Seetharaman J, Fadeel B, Star A, Shvedova AA (May 2010). "Carbon nanotubes degraded by neutrophil myeloperoxidase induce less pulmonary inflammation". Nature Nanotechnology. 5 (5): 354–9. Bibcode:2010NatNa...5..354K. doi:10.1038/nnano.2010.44. PMC 6714564. PMID 20364135.
- Clay Dillow (April 6, 2010). "Scientists Devise A Means For Human Bodies To Break Down Carbon Nanotubes". Popular Science.
- ^ a b c d Aratani Y (2018-02-15). "Myeloperoxidase: Its role for host defense, inflammation, and neutrophil function". Archives of Biochemistry and Biophysics. 640: 47–52. doi:10.1016/j.abb.2018.01.004. ISSN 0003-9861. PMID 29336940.
- ^ Hampton MB, Kettle AJ, Winterbourn CC (Nov 1998). "Inside the neutrophil phagosome: oxidants, myeloperoxidase, and bacterial killing". Blood. 92 (9): 3007–17. doi:10.1182/blood.V92.9.3007. PMID 9787133.
- ^ Davies MJ (February 2021). "Myeloperoxidase: Mechanisms, reactions and inhibition as a therapeutic strategy in inflammatory diseases". Pharmacology & Therapeutics. 218: 107685. doi:10.1016/j.pharmthera.2020.107685. PMID 32961264. S2CID 221865058.
- ^ a b Davey CA, Fenna RE (August 1996). "2.3 A resolution X-ray crystal structure of the bisubstrate analogue inhibitor salicylhydroxamic acid bound to human myeloperoxidase: a model for a prereaction complex with hydrogen peroxide". Biochemistry. 35 (33): 10967–10973. doi:10.1021/bi960577m. PMID 8718890.
- ^ Mathy-Hartert M, Bourgeois E, Grülke S, Deby-Dupont G, Caudron I, Deby C, et al. (April 1998). "Purification of myeloperoxidase from equine polymorphonuclear leucocytes". Canadian Journal of Veterinary Research. 62 (2): 127–132. PMC 1189459. PMID 9553712.
- ^ a b Davies MJ (January 2011). "Myeloperoxidase-derived oxidation: mechanisms of biological damage and its prevention". Journal of Clinical Biochemistry and Nutrition. 48 (1): 8–19. doi:10.3164/jcbn.11-006FR. PMC 3022070. PMID 21297906.
- ^ Shaw SA, Vokits BP, Dilger AK, Viet A, Clark CG, Abell LM, et al. (November 2020). "Discovery and structure activity relationships of 7-benzyl triazolopyridines as stable, selective, and reversible inhibitors of myeloperoxidase". Bioorganic & Medicinal Chemistry. 28 (22): 115723. doi:10.1016/j.bmc.2020.115723. PMID 33007547. S2CID 222145838.
- ^ Shin K, Hayasawa H, Lönnerdal B (Mar 2001). "Mutations affecting the calcium-binding site of myeloperoxidase and lactoperoxidase". Biochemical and Biophysical Research Communications. 281 (4): 1024–9. doi:10.1006/bbrc.2001.4448. PMID 11237766.
- ^ Flint SM, McKinney EF, Smith KG (Mar 2015). "Emerging concepts in the pathogenesis of antineutrophil cytoplasmic antibody-associated vasculitis". Current Opinion in Rheumatology. 27 (2): 197–203. doi:10.1097/BOR.0000000000000145. PMID 25629443. S2CID 20296651.
- ^ Frangie C, Daher J (2022-05-06). "Role of myeloperoxidase in inflammation and atherosclerosis (Review)". Biomedical Reports. 16 (6): 53. doi:10.3892/br.2022.1536. ISSN 2049-9434. PMC 9112398. PMID 35620311.
- ^ Brennan ML, Penn MS, Van Lente F, Nambi V, Shishehbor MH, Aviles RJ, Goormastic M, Pepoy ML, McErlean ES, Topol EJ, Nissen SE, Hazen SL (Oct 2003). "Prognostic value of myeloperoxidase in patients with chest pain". The New England Journal of Medicine. 349 (17): 1595–604. doi:10.1056/NEJMoa035003. PMID 14573731. S2CID 22084078.
- ^ Heslop CL, Frohlich JJ, Hill JS (Mar 2010). "Myeloperoxidase and C-reactive protein have combined utility for long-term prediction of cardiovascular mortality after coronary angiography". Journal of the American College of Cardiology. 55 (11): 1102–9. doi:10.1016/j.jacc.2009.11.050. PMID 20223364.
- ^ Leong AS, Cooper K, Leong, FJ (2003). Manual of Diagnostic Antibodies for Immunohistology. London: Greenwich Medical Media. pp. 325–326. ISBN 1-84110-100-1.
- ^ Csernok E, Moosig F (Aug 2014). "Current and emerging techniques for ANCA detection in vasculitis". Nature Reviews. Rheumatology. 10 (8): 494–501. doi:10.1038/nrrheum.2014.78. PMID 24890776. S2CID 25292707.
- ^ Kettle AJ, Gedye CA, Winterbourn CC (Jan 1997). "Mechanism of inactivation of myeloperoxidase by 4-aminobenzoic acid hydrazide". The Biochemical Journal. 321. 321 (2): 503–8. doi:10.1042/bj3210503. PMC 1218097. PMID 9020887.