User:Jlong74/sandbox
Neuronal Death in the PD brain | |
|---|---|
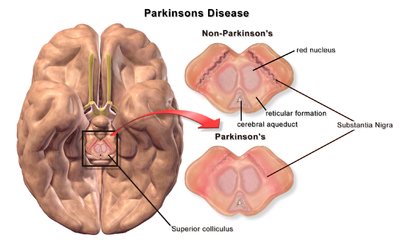 A brain without and with Parkinson's Disease compared in Substantia Nigra |
Neuronal Death in Parkinson's Disease
[edit]Neuronal Death in Parkinson's Disease is referring to the death of dopaminergic neurons as a result of changes in biological activity in the brain with respect to Parkinson's disease (PD). There are currently several mechanisms that are proposed to lead to neuronal death, however, not all of them are well understood. Five proposed major mechanisms for neuronal death in Parkinson's Disease include: Lewy Body formation, autophagy disruption, changes in cell metabolism or mitochondrial function, neuroinflammation or lastly blood-brain barrier (BBB) breakdown resulting in vascular leakiness.[1]
Protein Aggregation
[edit]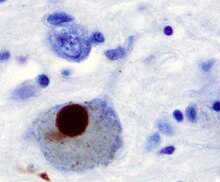
The first major proposed cause of neuronal death in Parkinson's Disease is due to proteins forming bundles called oligomers. The protein alpha-synuclein is known to be increased in the brains of Parkinson's Disease patients and aggregates to form Lewy bodies (shown to left). Traditionally, Lewy bodies were thought to be the main cause of cell death in Parkinson's Disease, however, it has more recently been suggested that Lewy bodies lead to other effects that cause cell death.[2] One thing for sure is that Lewy bodies are widely recognized as a pathological marker of Parkinson's disease. The following paragraph is an excerpt of the brain cell death section from the article Parkinson's Disease and briefly explains the mechanism by which alpha-synuclein causes neuronal death.
"One mechanism consists of an abnormal accumulation of the protein alpha-synuclein bound to ubiquitin in the damaged cells. This insoluble protein accumulates inside neurones forming inclusions called Lewy bodies. According to the Braak staging, a classification of the disease based on pathological findings, Lewy bodies first appear in the olfactory bulb, medulla oblongata and pontine tegmentum, with individuals at this stage being asymptomatic. As the disease progresses, Lewy bodies later develop in the substantia nigra, areas of the midbrain and basal forebrain, and in a last step the neocortex. These brain sites are the main places of neuronal degeneration in PD; however, Lewy bodies may not cause cell death and they may be protective. In people with dementia, a generalized presence of Lewy bodies is common in cortical areas. Neurofibrillary tangles and senile plaques, characteristic of Alzheimer's disease (AD), are not common unless the person is demented."
Autophagy Disruption
[edit]
The second major proposed mechanism for neuronal death in Parkinson's Disease, Autophagy, is a mechanism by which inner components of the cell are broken down and recycled for use.[2][3] Autophagy has been shown to play a role in brain health, helping to regulate cellular function. Disruption of the autophagy mechanism can lead to several different types of diseases like Parkinson's Disease.[3]
Autophagy can also clear aggregated protein, however, in neurodegenerative diseases autophagy sometimes can not break down and clear the oligomers fast enough to maintain regular cell function. Without clearence of protein bundles or other harmful molecules, cells start to alter their function and eventually undergo cell death.[4]
Autophagy dysfunction in Parkinson's Disease has also been shown to lead to dysregulated mitochondria degradation.[5]
Changes in Cell Metabolism
[edit]
The third major proposed cause of cell death in Parkinson's Disease involves an organelle that is often referred to as the "powerhouse" of the cell, the mitochondria. This is an accurate analogy because mitochondria are responsible for providing much of the energy required in a cell for it to function. In Parkinson's Disease, it has been shown that mitochondrial function is disrupted, causing cells to become malnourished and die.[6][7]
The mechanism behind mitochondrial dysfunction in Parkinson's Disease is hypothesized to be the PINK1 and Parkin complex which has been shown to drive autophagy of the mitochondria, also known as mitophagy.[6][7][8] PINK1 is a protein that is normally transported into the mitochondria, but can also accumulate on the surface of impaired mitochondria. Accumulated PINK1 then recruits Parkin which initiates the break down of dysfunctional mitochondria, a mechanism that acts as a "quality control"[6] In Parkinson's Disease, the genes coding PINK1 and Parkin are thought to be mutated, therefore preventing the breakdown of impaired mitochondria, causing abnormal function and morphology of mitochondria and eventually cell death[6][7] Mitochondrial DNA (mtDNA) mutations have also been shown to accumulate with age[9] indicating that susceptibility to this mechanism of neuronal death increases with age.
Another mitochondrial-related mechanism for cell death in Parkinson's Disease is the generation of Reactive Oxygen Species (ROS).[9][10] ROS are highly reactive molecules that contain oxygen and can disrupt functions within the mitochondria and the rest of the cell. With increasing age, mitochondria lose their ability to remove ROS yet still maintain their production of ROS, causing an increase in net production of ROS and eventually cell death.[9][10]
Neuroinflammation
[edit]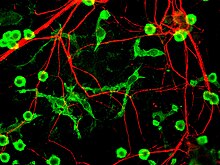
The fourth proposed major mechanism of neuronal death in Parkinson's Disease, Neuroinflammation, is generally understood for neurodegenerative diseases, however, specific mechanisms are not completely characterized for PD.[11] One major cell type involved in neuroinflammation is the microglia. The following paragraph is an excerpt from the Microglia section of the article Neuroinflammation.
"Microglia are recognized as the innate immune cells of the central nervous system. Microglia actively survey their environment through, and change their cell morphology significantly in response to neural injury. Acute inflammation in the brain is typically characterized by rapid activation of microglia. During this period, there is no peripheral immune response. Over time, however, chronic inflammation causes the degradation of tissue and of the blood–brain barrier. During this time, microglia generate reactive oxygen species and release signals to recruit peripheral immune cells for an inflammatory response."
In addition, microglia are known to have two major states: one is called M1, a state in which cells are activated and secrete pro-inflammatory factors and the other is called M2, a state in which cells are deactivated and secrete anti-inlfammatory factors.[12] Microglia are usually in their resting state (M2), but in Parkinson's Disease can be activated (M1) by bundles of alpha-synuclein protein called oligomers. The M1 microglia release pro-inflammatory factors which can cause motor neurons to die. In this case, dying cells can release factors to increase the activation of M1 microglia, leading to a positive feedback loop which causes continually increasing cell death.[11]
BBB Breakdown
[edit]
The fifth proposed major mechanism for cell death is the breakdown of the Blood-Brain Barrier (BBB). The BBB has three cell types that tightly regulate the flow of molecules in and out of the brain: endothelial cells, pericytes and astrocytes. In neuro-degenerative diseases, BBB breakdown has been measured and identified in specific regions of the brain such as the substantia nigra in Parkinson's Disease and hippocampus in Alzheimer's Disease.[13] It has been proposed that protein aggregates or cytokines from neuroinflammation interfere with cell receptors and alter their function in the BBB.[13][14] Most notably, Vascular Endothelial Growth Factor (VEGF) and VEGF receptors are thought to be disregulated in neurodegenerative diseases. The interaction between this protein and its receptors leads to cell proliferation, but is believed to be disrupted in Parkinson's Disease and Alzheimer's Disease.[14][15] This then causes cells to stop growing and therefore, prevents new capillary formation via angiogenesis. Cell receptor disruption can also affect the ability for cells to adhere to one another with adherens junctions.[16]
Without new capillary formation, the existing capillaries breakdown and cells start to dissociate from each other. This in turn leads to the breakdown of gap junctions.[17][18] Gap junctions in endothelial cells in the BBB help prevent large or harmful molecules from entering the brain by regulating the flow of nutrients to the brain. However, as gap junctions breakdown, plasma proteins are able to enter the brain extracellular matrix.[17] This mechanism is also known as vascular leakiness, where capillary degeneration leads to blood and blood proteins "leaking" into the brain. Vascular leakiness can eventually cause neurons to alter their function and shift towards apoptotic behavior or cell death.
Impact on Locomotion
[edit]
Dopaminergic Neurons are the most abundant type of neuron in the Substantia Nigra, a part of the brain that has much to do with motor control/learning. Dopamine is a neurotransmitter which is used to activate motor neurons in the brain (central nervous system). The activated motor neurons then transmit their signals, via action potential, to motor neurons in the legs to allow control for walking (Peripheral Nervous System).[19] However, when a significant percentage of the motor neurons die (about %50-%60), this decreases up to %80 of the dopamine levels[7] which inhibits the ability for neurons to generate and transmit a signal. This transmission inhibition ultimately causes Parkinsonian Gait with symptoms such as hunched and slowed walking or tremors.
Understanding these major proposed causes of cell death is vital to finding a cure for Parkinson's Disease and other neurodegenerative diseases. Neuronal death in neurodegenerative diseases, though not completely understood, can provide a promising avenue for research in reversing the effects of Parkinson's Disease.
References
[edit]- ^ Tansey, M. G., & Goldberg, M. S. (2010). Neuroinflammation in Parkinson's disease: Its role in neuronal death and implications for therapeutic intervention. Neurobiology of Disease, 37(3), 510-518. doi:10.1016/j.nbd.2009.11.004
- ^ a b Schapira, A. H. (2009). Etiology and Pathogenesis of Parkinson Disease. Neurologic Clinics, 27(3), 583-603. doi:10.1016/j.ncl.2009.04.004
- ^ a b Stern, S. T., & Johnson, D. N. (2008). Role for nanomaterial-autophagy interaction in neurodegenerative disease. Autophagy, 4(8), 1097-1100. doi:10.4161/auto.7142
- ^ Ghavami, S., Shojaei, S., Yeganeh, B., Ande, S. R., Jangamreddy, J. R., Mehrpour, M., . . . Łos, M. J. (2014). Autophagy and apoptosis dysfunction in neurodegenerative disorders. Progress in Neurobiology, 112, 24-49. doi:10.1016/j.pneurobio.2013.10.004
- ^ Hu, Z., Yang, B., Mo, X., & Xiao, H. (2014). Mechanism and Regulation of Autophagy and Its Role in Neuronal Diseases. Molecular Neurobiology Mol Neurobiol, 52(3), 1190-1209. doi:10.1007/s12035-014-8921-4
- ^ a b c d Chen, H., & Chan, D. C. (2009). Mitochondrial dynamics-fusion, fission, movement, and mitophagy-in neurodegenerative diseases. Human Molecular Genetics, 18(R2). doi:10.1093/hmg/ddp326
- ^ a b c d Pickrell, A., & Youle, R. (2015). The Roles of PINK1, Parkin, and Mitochondrial Fidelity in Parkinson’s Disease. Neuron, 85(2), 257-273. doi:10.1016/j.neuron.2014.12.007
- ^ Narendra, D., Tanaka, A., Suen, D., & Youle, R. J. (2008). Parkin is recruited selectively to impaired mitochondria and promotes their autophagy. J Cell Biol The Journal of Cell Biology, 183(5), 795-803. doi:10.1083/jcb.200809125
- ^ a b c Lin, M. T., & Beal, M. F. (2006). Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature, 443(7113), 787-795. doi:10.1038/nature05292
- ^ a b Jomova, K., Vondrakova, D., Lawson, M., & Valko, M. (2010). Metals, oxidative stress and neurodegenerative disorders. Molecular and Cellular Biochemistry Mol Cell Biochem, 345(1-2), 91-104. doi:10.1007/s11010-010-0563-x
- ^ a b Glass, C. K., Saijo, K., Winner, B., Marchetto, M. C., & Gage, F. H. (2010). Mechanisms Underlying Inflammation in Neurodegeneration. Cell, 140(6), 918-934. doi:10.1016/j.cell.2010.02.016
- ^ Zlokovic, B. V. (2008). The Blood-Brain Barrier in Health and Chronic Neurodegenerative Disorders. Neuron, 57(2), 178-201. doi:10.1016/j.neuron.2008.01.003
- ^ a b Zlokovic, B. V. (2011). Neurovascular pathways to neurodegeneration in Alzheimer's disease and other disorders. Nature Reviews Neuroscience Nat Rev Neurosci. doi:10.1038/nrn3114
- ^ a b Hao, T., & Rockwell, P. (2013). Signaling through the vascular endothelial growth factor receptor VEGFR-2 protects hippocampal neurons from mitochondrial dysfunction and oxidative stress. Free Radical Biology and Medicine, 63, 421-431. doi:10.1016/j.freeradbiomed.2013.05.036
- ^ Almodovar, C. R., Lambrechts, D., Mazzone, M., & Carmeliet, P. (2009). Role and Therapeutic Potential of VEGF in the Nervous System. Physiological Reviews, 89(2), 607-648. doi:10.1152/physrev.00031.2008
- ^ Förster, C., Burek, M., Romero, I. A., Weksler, B., Couraud, P., & Drenckhahn, D. (2008). Differential effects of hydrocortisone and TNFα on tight junction proteins in an in vitro model of the human blood-brain barrier. The Journal of Physiology, 586(7), 1937-1949. doi:10.1113/jphysiol.2007.146852
- ^ a b Nagasawa, K., Chiba, H., Fujita, H., Kojima, T., Saito, T., Endo, T., & Sawada, N. (2006). Possible involvement of gap junctions in the barrier function of tight junctions of brain and lung endothelial cells. J. Cell. Physiol. Journal of Cellular Physiology, 208(1), 123-132. doi:10.1002/jcp.20647
- ^ Marambaud, P., Dreses-Werringloer, U., & Vingtdeux, V. (2009). Calcium signaling in neurodegeneration. Molecular Neurodegeneration Mol Neurodegeneration, 4(1), 20. doi:10.1186/1750-1326-4-20
- ^ Barnett MW, Larkman PM; Larkman (June 2007). "The action potential". Pract Neurol 7 (3): 192–7. PMID 17515599

